
What is Intracranial Hypertension?
Intracranial pressure (ICP)
Types of IH
Causes and symptoms
Idiopathic intracranial hypertension
Case report
Diagnosis and treatment
References
Further reading
Intracranial hypertension (IH), a clinical condition typically seen in the intensive care unit, is caused by increased pressure surrounding the brain. In many situations, the cause of chronic IH is unknown, referred to as idiopathic IH (IIH).
It can be caused by a primary central nervous system (CNS) lesion or a consequence of another systemic condition. It leads to poor outcomes, including increased mortality.
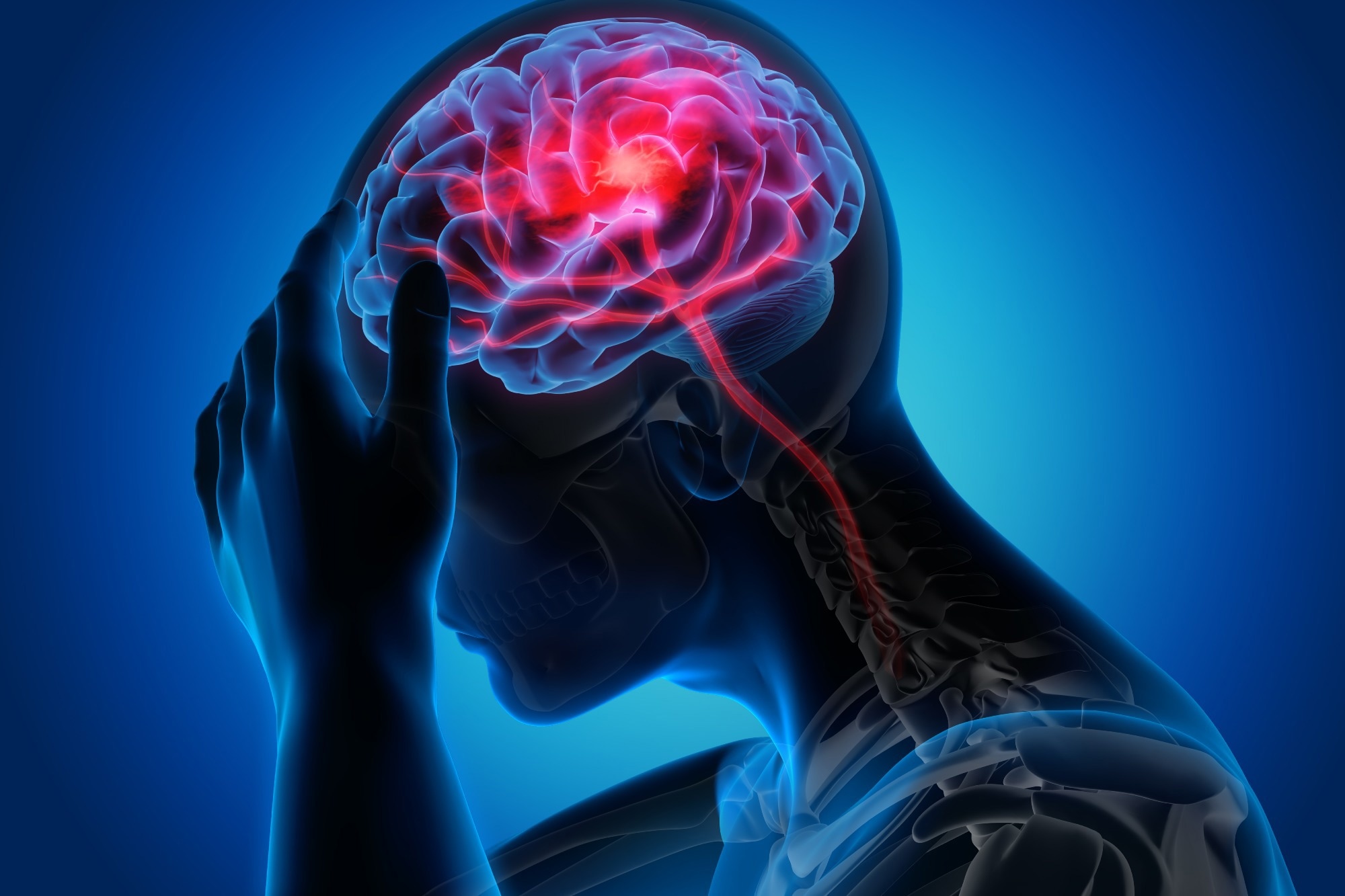 Image Credit: peterschreiber.media/Shutterstock.com
Image Credit: peterschreiber.media/Shutterstock.com
Intracranial pressure (ICP)
The normal intracranial pressure in adults is less than 15 mm Hg, with brief rises related to coughing or sneezing.
Sustained intracranial pressure values exceeding 20 mm Hg are considered pathogenic and should be treated aggressively in patients with traumatic brain damage. Intracranial volume and intracranial pressure have an exponential connection.
Pressure initially rises slightly with increasing volume, but when the system's buffering capabilities are exhausted, ICP can rise significantly. Intracranial and systemic events lead to increased intracranial pressure following traumatic brain injury.
In clinical practice, invasive and non-invasive ICP monitoring methods estimate the appropriate cerebral perfusion pressure (CPP).
Types of IH
Intracranial hypertension can be acute or chronic; Acute IH can happen unexpectedly due to a severe head injury, stroke, or brain abscess, and the rare chronic type can be long-lasting with no known cause at times.
Idiopathic IH (pseudotumor cerebri) is characterized by elevated intracranial pressure with no apparent etiology.
Causes and symptoms
Intracranial hypertension can occur due to several conditions caused by potential mechanisms, including venous blockage, cerebral edema, and increased brain and blood volume.
Chronic intracranial hypertension can occur due to a blood clot (on the brain's surface), tumor, or infection in the brain (meningitis).
IH can be caused by both primary and secondary brain injury (SBI) and has variable clinical symptoms. Headache, nausea, and vomiting, as well as diplopia, papilledema, and pupillary dilatation, are common symptoms.
Severe hypertension, bradycardia, and irregular breathing are also possible. A potentially fatal consequence of IH is brain herniation. Many kinds of brain herniation, such as uncal transtentorial, subfalcine, tonsilar, and transcalvarial herniation, can be seen in these patients.
Idiopathic intracranial hypertension
Idiopathic intracranial hypertension is defined by signs and symptoms of elevated ICP with no known cause.
The condition is linked to obesity, and most patients are female (typically of reproductive age). Headaches (sometimes mimicking migraine or tension-type headaches), vision impairment (leading to sight loss), pulsatile tinnitus, and back pain are common symptoms of idiopathic intracranial hypertension.
The clinical presentation is widely diverse and can lead to delays in diagnosis. The condition is extremely rare, with an annual incidence of 0.9 per 100,000 people. In young obese women, the incidence increases drastically and affects 19 per 100,000.
The underlying pathophysiology is unknown; however, numerous aetiologies have been proposed. Obesity is linked to increased intraabdominal and intrapleural pressure, which can reduce CSF outflow by increasing venous pressure and raising ICP. Sleep apnea can also cause increased ICP due to hypercarbia and vasodilation.
Case report
They presented a 43-year-old man who reported recurring pain around his right eye. The pain began around 5-6 weeks before admission, described as pressure-like, with a severity rating of 7/10.
The agony lasted about 10 minutes and then disappeared, with episodes occurring three to four times a day. The patient denied that there were any triggering causes. The patient was unaware of trigger points.
The patient denied experiencing any changes in speech, vision, balance, sensation, or strength. Tinnitus, hearing loss, photophobia, phonophobia, nausea, and vomiting were all denied by him. A recent CT chest indicated bronchiectasis, and the patient had recently received antibiotics for a respiratory tract infection.
He gained roughly 18 kg during the last few months. Prior medical history involves nasal polyps, diabetes, obesity, hypertension, and smoking. The patient appeared obese but healthy on general physical examination, with no abnormalities observed on cardiovascular, respiratory, or abdominal exams.
On neurologic assessment, his cranial nerves were found to be slightly asymmetric. The patient's symptoms resolved completely. His checkup was normal following the lumbar puncture, and he was started on acetazolamide 500 mg twice daily. The patient was asymptomatic three months later, with no negative effects from the treatment.
The sixth cranial nerve is frequently involved in IIH. However, the involvement of other cranial nerves is uncommon in this condition. They described a patient with IIH who had episodic unilateral retro-orbital pain and various cranial nerve anomalies without papilledema.
Imaging examinations ruled out other possibilities, and the fast relief of symptoms upon lumbar puncture confirmed that they were caused by intracranial hypertension. Atypical manifestations of such a severe yet manageable condition must be identified and addressed.
Diagnosis and treatment
A CT Scan, an MRI scan, a lumbar puncture, and assessments of eyes and vision can aid in establishing IH in a patient. The goal of treatment is to lower intracranial pressure, ease headaches, and maintain vision. Nonsurgical treatments include weight loss, acetazolamide, and topiramate as first-line therapy modalities.
According to the most recent traumatic brain injury recommendations, the primary goal of IH treatment is to keep ICP below 22 mmHg and CPP over 60 mmHg. Achieving these goals could make the difference between life and death for the brain.
The therapeutic measures for IH are divided into general preventative measures and those used in the acute period to reduce ICP and optimize CPP.
Progress in monitoring and understanding the pathophysiological mechanisms of IH enables the introduction of targeted therapies to enhance these patients' outcomes.
Although therapy for the fundamental cause of IH is the basic first approach, all efforts in the ICU should be directed against preventing SBI.
References
- Miah, L., Strafford, H., Fonferko-Shadrach, B., Hollinghurst, J., Sawhney, I. M., Hadjikoutis, S., Rees, M. I., Powell, R., Lacey, A., & Pickrell, W. O. (2021). Incidence, Prevalence and Healthcare Outcomes in Idiopathic Intracranial Hypertension: A Population Study. Neurology, 96(8), e1251–e1261. Advance online publication. https://doi.org/10.1212/WNL.0000000000011463
- Schizodimos, T., Soulountsi, V., Iasonidou, C., & Kapravelos, N. (2020). An overview of management of intracranial hypertension in the intensive care unit. Journal of anesthesia, 34(5), 741–757. https://doi.org/10.1007/s00540-020-02795-7
- Toscano, S., Lo Fermo, S., Reggio, E., Chisari, C. G., Patti, F., & Zappia, M. (2021). An update on idiopathic intracranial hypertension in adults: a look at pathophysiology, diagnostic approach and management. Journal of neurology, 268(9), 3249–3268. https://doi.org/10.1007/s00415-020-09943-9
- Kalyvas, A., Neromyliotis, E., Koutsarnakis, C., Komaitis, S., Drosos, E., Skandalakis, G. P., Pantazi, M., Gobin, Y. P., Stranjalis, G., & Patsalides, A. (2021). A systematic review of surgical treatments of idiopathic intracranial hypertension (IIH). Neurosurgical review, 44(2), 773–792. https://doi.org/10.1007/s10143-020-01288-1
- Mollan, S. P., Aguiar, M., Evison, F., Frew, E., & Sinclair, A. J. (2019). The expanding burden of idiopathic intracranial hypertension. Eye (London, England), 33(3), 478–485. https://doi.org/10.1038/s41433-018-0238-5
- Markey, K. A., Mollan, S. P., Jensen, R. H., & Sinclair, A. J. (2016). Understanding idiopathic intracranial hypertension: mechanisms, management, and future directions. The Lancet. Neurology, 15(1), 78–91. https://doi.org/10.1016/S1474-4422(15)00298-7
- Wakerley, B. R., Tan, M. H., & Ting, E. Y. (2015). Idiopathic intracranial hypertension. Cephalalgia : an international journal of headache, 35(3), 248–261. https://doi.org/10.1177/0333102414534329
- Stocchetti, N., & Maas, A. I. (2014). Traumatic intracranial hypertension. The New England journal of medicine, 370(22), 2121–2130. https://doi.org/10.1056/NEJMra1208708
Further reading
- Intracerebral Hemorrhage (ICH) Research and Clinical Trials
- What is a Stroke?
- The Quest for an Acute Traumatic Brain Injury Treatment
Last Updated: Sep 5, 2023