At least 10 million South Africans didn’t have enough food or money to buy food in 2019, according to the country’s statistics agency. This food insecurity remains a leading health problem that is unlikely to be eradicated any time soon.
To support those affected, it’s important to understand how South African households cope with food insecurity. Existing research on this has been conducted sub-nationally. The focus has mostly been on the poorest regions of the country. The national picture of household food insecurity has not been clear.
Another gap in understanding has been the impact of households’ coping strategies on mental health. Such strategies include eating less, borrowing or using credit, and even begging for food on the streets.
Our recent study investigated food insecurity and related coping strategies among South African households and their association with anxiety and depression.
We have shown, for the first time, how the strategies that South African households commonly use to cope with food insecurity are associated in different ways with anxiety and depression. In other words, some coping strategies may have a greater impact than others on mental health. Our findings suggest that begging for food was the most harmful coping strategy for mental health. Conversely, relying on less preferred and less expensive foods was less associated with anxiety and depression.
The poor are the most food insecure
For our study, we conducted face-to-face interviews with a nationally representative sample of 3,402 adults in October 2021. The survey data was statistically weighted to represent over 39 million South African households.
We assessed food insecurity using the Community Childhood Hunger Identification Project questionnaire. This survey tool allowed us to categorize the households into three groups: food secure, at risk, and food insecure.
We found that over 20% (1 in 5) of the South African households were food insecure. But the prevalence varied widely across the provinces. The Eastern Cape province was the most affected (32% of households there were food insecure). We also confirmed that food access in South Africa largely depends on socio-economic status. People who are uneducated, the unemployed and those receiving a low monthly income are the most severely affected by inadequate food access.
Food insecurity was most common among colored people (24%)—people of mixed European, African or Asian ancestry. Black people (23%) were also more food insecure than white (5%) and Asian (4%) categories. These large differences in food insecurity rates have been attributed to former apartheid regime policies. These policies led to racial discrimination, geographic segregation, and other unsustainable settlement patterns. Hence, solutions to such inequalities require fundamental restructuring of the South African economy.
Many households beg for food
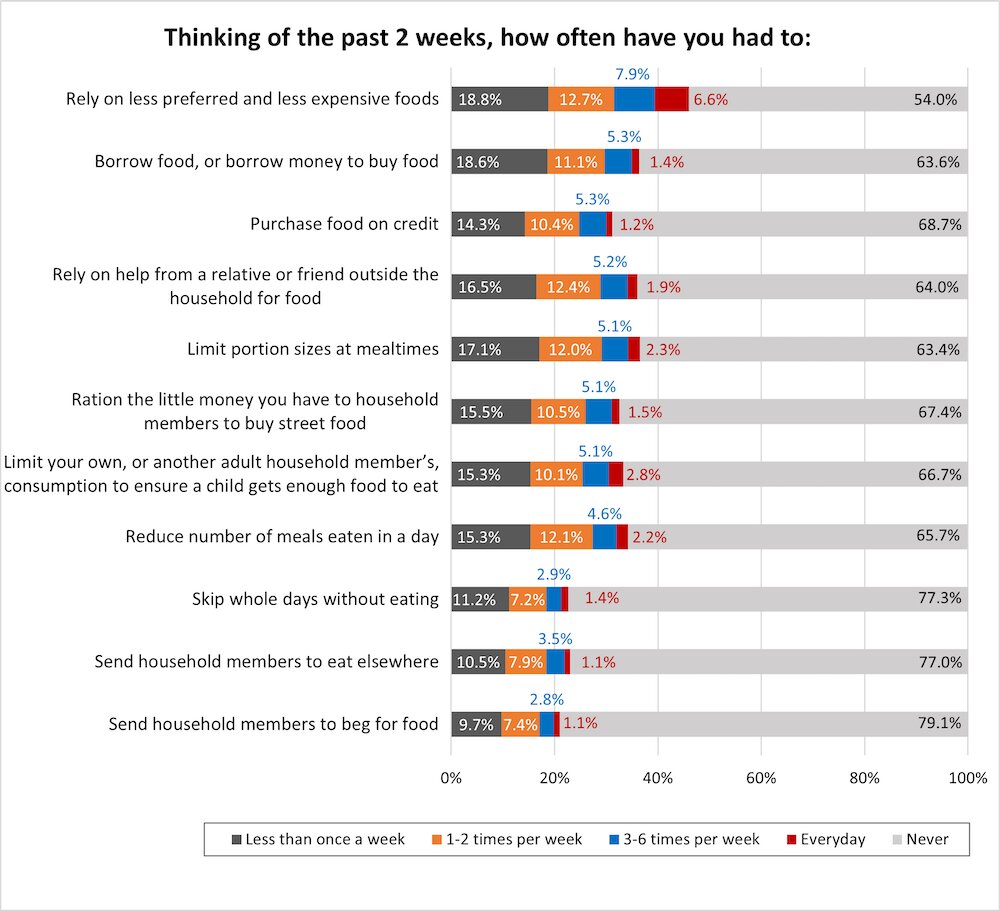
We used the Coping Strategies Index questionnaire to assess the extent to which South African households used harmful coping strategies when faced with food insecurity.
All coping strategies were used to some extent. The most common strategy (used by at least 46%) was relying on less preferred and less expensive foods. Sending household members to beg for food was the least common strategy. It was used by almost 21% (more than 1 in 5) of the households. We didn’t expect this high rate of households begging for food. Begging is a strategy often used by homeless people, and it’s sometimes seen as socially unacceptable.
The impact on mental health
To assess the risk of impaired mental health among the household respondents, we used the General Anxiety Disorder-7 and Patient Health Questionnaire-9 questionnaires. These are validated tools for screening symptoms of anxiety and depression, respectively.
Our findings demonstrated that living in a food insecure household was associated with a higher risk of anxiety and depression. One level increase in food insecurity (shifting from the “food secure” to the “at risk” or from the “at risk” to “food insecure”) was associated with being 1.7 times more likely to experience higher levels of anxiety or depression.
Those who were using the strategy of begging for food were 2.3 times more likely to experience higher levels of anxiety and depression. This confirms what has been recently suggested by several studies: that an increase in food insecurity and depressive symptoms during COVID-19 may be related.
For example, the National Income Dynamics Study—Coronavirus Rapid Mobile Survey reported that the rise in food insecurity during COVID-19 lockdowns was accompanied by an increased rate of people screening positive for depressive symptoms.
Finding solutions
Overall, our study suggested that food insecurity in South Africa remains a major health problem. And poorer households are disproportionately affected. Living in a food insecure household may be forcing poor South Africans to use a variety of coping strategies that ultimately lead to anxiety and depression.
Our report is timely in light of the recent announcement by the South African government that it would prioritize the issues of unemployment, poverty and inequality. In the 2022 State of the Nation Address the president stated that there would be several fundamental reforms primarily aimed at reviving economic growth. This would ultimately assist in combating high employment and food insecurity rates.
Given our new findings, food insecurity and related coping strategies should be considered as risk factors for impaired mental health. The proposed public measures to reduce high rates of food insecurity and unemployment may assist households in choosing less harmful coping strategies and ultimately improve the mental health quality of South Africans.
Provided by
The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Source: Read Full Article