Researchers from the University of Oxford, U.K., have investigated the evolution of antibiotic resistance properties of antimicrobial peptides (AMPs). In the paper “The evolution of colistin resistance increases bacterial resistance to host antimicrobial peptides and virulence,” published in eLife, researchers detail a disturbing discovery of how a specific type of antimicrobial agent, colistin, could be training E. coli and possibly other pathogens to evade the human immune system better.
Antimicrobial peptides (AMPs) are multifunctional molecules found in all life forms and are an essential part of the innate immune system of animals. AMPs modulate immune responses and defend against invading pathogens by killing bacteria, yeasts, fungi and viruses and can even attack cancer cells. AMPs are evolutionarily deeply conserved molecules in organisms ranging from prokaryotes to humans.
This highly conserved, naturally trained aspect of AMPs is likely why they are so successful in fighting off otherwise resistant pathogens and the primary cause for concern in the study. If anthropogenic use of AMPs can drive the resistance to AMPs as a treatment, it could also be driving the evolution of cross-resistance to the innate immune system of humans and animals.
According to the United Nations Environment Program (UNEP), antimicrobial resistance is a growing global threat. While antimicrobials have been a go-to method of preventing death from all sorts of infections, their effectiveness is now in jeopardy as treatments that once worked reliably no longer do because microorganisms have built resistance to them.
Colistin is an AMP derived from a bacillus bacteria once used widely in agriculture beginning in the 1980s. After a breakout of colistin-resistant E. coli in China, the practice was banned in 2016. Colistin is now primarily used for severe infections resistant to multiple other antibiotics. It is a last line of defense when other options have failed, so the pathogenic evolution of resistance to colistin would have terrible consequences. What the researchers found in their study hints at something far worse.
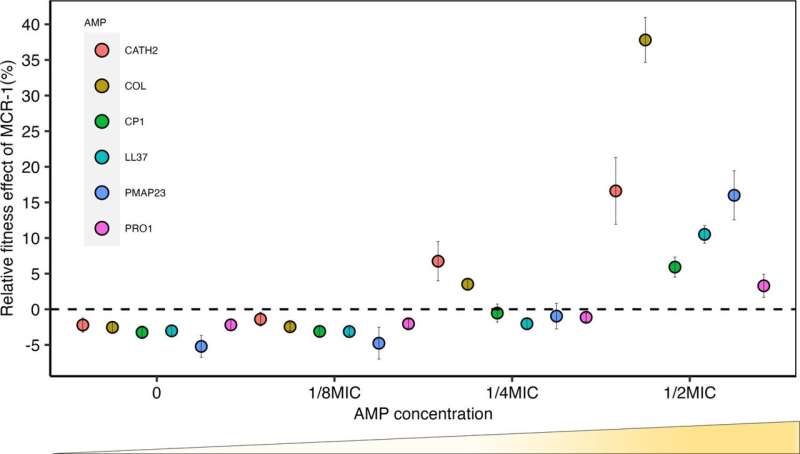
The researchers tested E. coli with colistin resistance gene MCR-1 against human and animal AMPs and found, on average, that MCR plasmids provided increased resistance to host AMPs by 62%.
In a blood serum experiment, the researchers found high levels of resistance to human serum, showing that MCR-1 effectively protects against even complex mixtures of antimicrobials. The team further isolated the experiment with a version of the tested strain that lacked MCR-1 (via gene knockout) and found it to behave like a wild type, pointing to the colistin-resistant MCR-1 gene as the driver of the resistance.
The results raise the possibility that increased AMP resistance provided by MCR-1 could increase bacterial invasion of hosts by compromising their innate immunity. If left unchecked, the loss of a critical therapeutic defense against multi-resistant pathogens that acquire AMP-resistant genes could impact clinical practitioners’ ability to combat them effectively. There is perhaps an even greater risk that “normal” pathogens, currently fought off by our innate immune system, could become immune to us.
More information:
Pramod K Jangir et al, The evolution of colistin resistance increases bacterial resistance to host antimicrobial peptides and virulence, eLife (2023). DOI: 10.7554/eLife.84395
Journal information:
eLife
Source: Read Full Article
