A team of investigators at the University of Chicago (Ill.), has devised a new scoring system that helps surgeons across surgical specialties decide when to proceed with medically necessary operations in the face of the resource constraints and increased risk posed by the Coronavirus Disease 2019 (COVID-19) pandemic. The process, called Medically Necessary Time-Sensitive (MeNTS) Prioritization, is published as an “article in press” on the Journal of the American College of Surgeons website ahead of print.
In the midst of the COVID-19 pandemic, hospitals must make sure they can care for the influx of patients who have advanced viral infection and therefore may require intensive care and the use of ventilators. Hospitals also must ensure that physicians, nurses, and other staff are not subjected to unnecessary risk of infection. At the same time, some patients that are not currently hospitalized still need surgical care that should be delayed for an excessive amount of time.
Decisions to proceed with MeNTS surgery at the present time are being made on a case-by-case basis, with surgeons following guidelines developed by individual surgical specialties, such as triaging breast cancer surgery recommendations developed by the COVID-19 Pandemic Breast Cancer Consortium 1 and released on April 14. Prior to that release, ACS released an overall recommendation 2 on March 13 that hospitals, health systems, and surgeons plan to minimize, postpone, or cancel elective operations until it is clear that the health care infrastructure can support critical care needs. This recommendation was followed by another more detailed guidance document released by ACS 3 on March 17 to aid in surgical decision making in triaging operations that features an Elective Surgery Acuity Scale (ESAS) from St. Louis University.
The new methodology described by University of Chicago surgeons addresses what many call “elective” surgical procedures and is designed to guide both surgeons within a specialty and OR leaders across different specialties. “The majority of surgical procedures are done because of disease processes that do not have good nonsurgical treatment options. If you delay these procedures, that itself can lead to problems and complications. If cancer surgery is postponed indefinitely, for example, there is the potential risk that the disease will become more advanced.
“If a patient has pain in the hip or knee, the additional restrictions on mobility, not to mention the pain itself, are real issues. Although we talk about these operations as being ‘elective,’ that doesn’t mean they are optional. It’s just a matter of the surgeon and the patient having the opportunity to elect the time when the operation should take place. The procedures are more aptly called medically-necessary and time-sensitive,” explained Vivek N. Prachand, MD, FACS, lead author of the article, and professor of surgery and chief quality officer at University of Chicago Medicine and Biological Sciences.
The MeNTS Prioritization process was created by a team of six representatives from general surgery, vascular surgery, surgical oncology, transplantation, cardiac surgery, otolaryngology, and surgical ethics. The team reviewed studies of the effect of COVID-19 as well as severe acute respiratory syndrome on hospital resources, health care providers, surgical procedures, and surgical patients in Asia and Europe and identified 21 factors related to outcome, risk of viral transmission to health care professional, and use of resources.
“We studied how patients undergoing surgery might potentially be at increased risk of postoperative problems if they had COVID-19. We looked at surgical procedures individually and whether these operations routinely require an ICU stay; other currently scarce hospital resources; and/or general anesthesia, which increases the risk for spreading the virus to the health care team. We also thought about the disease process itself: how effective are non-surgical options? Would a wait of two weeks or six weeks make the operation riskier or more difficult to perform and increase the chance a patient might have complications or have to stay in the hospital longer?” Dr. Prachand added.
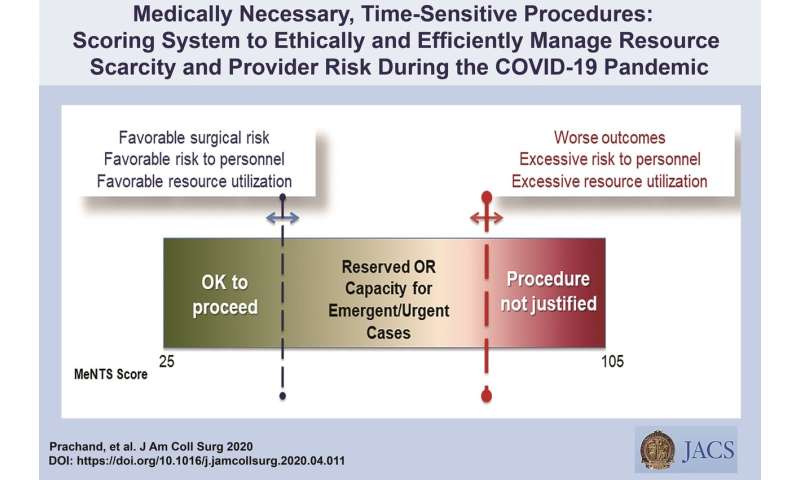
Each of the 21 factors is scored on a scale of 1 to 5, and the total score, ranging from 21 to 105, is computed for each case. The higher the score, the greater the risk to the patient, the higher the utilization of health care resources, and the higher the chance of viral exposure to the health care team. (See the linked sample MeNTS worksheet for a full list of the factors that are scored.)
University of Chicago surgeons have been using MeNTS for about two weeks, and they have increased the number of medically necessary, time-sensitive operations to about 15 per day, including colon resection for a painful bleeding cancer, removal of an infected hip replacement, urgent stereotactic brain biopsy of a relatively quickly growing diffuse brain tumor, and repair of a lacerated finger tendon.
The scoring system has been welcomed by University of Chicago specialties not originally involved in its creation, such as orthopedics, gynecology, and anesthesiology. “The MeNTS process gives our anesthesiology colleagues more reassurance that we are taking into consideration their risk in the care of certain patients. It also helps surgical trainees understand that decisions are being made in an equitable and transparent way,” Dr. Prachand said.
Source: Read Full Article
