People with Down syndrome are more likely than the general population to develop serious respiratory infections. Often, symptoms are so severe that patients require hospitalization. As respiratory season moves in, researchers on campus are working to understand what unique genetic factors may contribute to this problem.
“Down syndrome is caused by the triplication of chromosome 21, and we really don’t fully understand the extent of how it impacts lung biology,” said Brian Niemeyer, Ph.D., research associate with the Linda Crnic Institute for Down Syndrome at the University of Colorado School of Medicine. “We know the immune system doesn’t function as well among individuals with Down syndrome, and we know there are some physical differences in the basic structure of their airways.”
Teasing out the reasons why may help researchers discover new strategies for preventing and treating these infections. Niemeyer and colleagues published a study in the journal iScience that analyzed differences in the lungs of those with Down syndrome.
The study assessed two main areas:
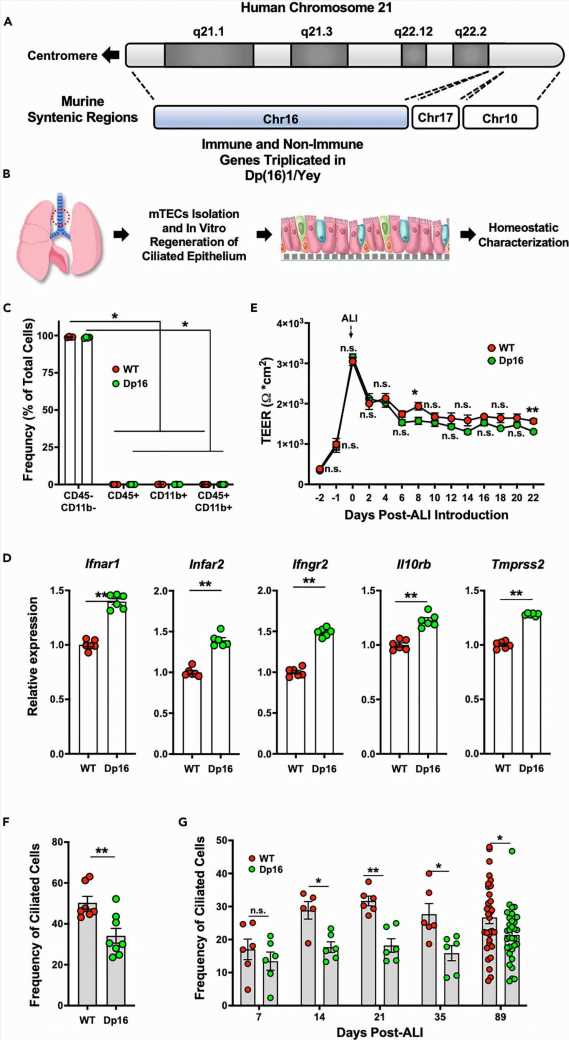
- how normal lung biology changes using a model of Down syndrome. Researchers examined how the distribution of cell types in the lung and length of cell function change homeostasis (stability in physical processes). This first part was done without any virus exposure.
- how the cells from the Down syndrome model respond after they have been exposed to a respiratory virus, like influenza.
These two approaches helped researchers see how the cells look normally and how they look when responding to a live infection.
Niemeyer, the study’s co-lead author, shared more about his team’s findings and their implications in the Q&A below.
How did your team conduct the study?
We used mouse models of airways. People have many different types of cells in their lungs. Some are called ciliated cells, which are responsible for knocking out any debris or pathogens that enter the lung.
Other cell types secrete mucus, which plays a big role in trapping pathogens and maintaining a healthy lung. To recreate the most basic aspects of lung architecture outside of the body, we grew these cells in something called an air-liquid interface using a cell culture device known as a transwell insert. The cells are grown on a thin, porous membrane where the bottom half is submerged in media, which supplies nutrients, and the top half is exposed to air. Using this culture method, you can study the different types of airway epithelial cells outside of the body.
Is it possible to use human cells for this research?
Ideally, it would be wonderful, but it’s a little invasive. We get the cells through bronchial brushings, and that can be a bit hard on an individual. Before taking that step, we wanted to prove the merits of this system and the study using a widely accepted mouse model of Down syndrome.
What were your main findings?
They included the following:
- We found a significant reduction in the frequency of ciliated cells in the Down syndrome airway model. We looked at a whole battery of measurements for how these cells function and behave normally. In addition to frequency, we also looked at how ciliated cells “beat.” The cilia on the ends of these cells beat back and forth, and that’s how they clear mucus buildup, particles, debris and dust out of the lung. The combination of fewer of these cells and a defect in their functions suggests there can be a problem with that process.
- We took videos of the cells and recorded them as the cilia were beating back and forth in order to measure the beating in cells. We found that the cells from the Down syndrome were beating at a slower rate.
- Even without any exposure to a virus, cells from the Down syndrome model appear to have deficiencies in the basic function of the lung. If cells aren’t even functioning well at baseline, that could help explain why they’re not responding well to infection.
- After exposure to influenza, we found that the cells from the Down syndrome model were hyper-responsive to infection when compared to control cells. They produced more inflammatory proteins despite showing the same amount of virus shedding.
Did the results show other reasons why people with Down syndrome have such severe infections?
We didn’t see any difference between the amount of virus that was produced in the Down syndrome model when compared to controls. Despite that, the cells from the Down syndrome model had an excessive immune system response aimed at fighting the infection. If your immune system is too activated, it can cause a lot of collateral damage in healthy cells while trying to clear the infection.
Are you doing future research on this topic?
Yes. We will be looking at how these immune cells actually impact the infected space. For example, we would like to see if the recruited immune cells cause differing levels of collateral damage in Down syndrome. Our work is a stepping-stone to better understand the biology of respiratory infections. It’s helping clarify what’s going on so we know what to target with treatments.
What are possible treatments?
We could inhibit immune cell recruitment, but before we use that as a treatment, we need more information about its impact. The immune cells may or may not be contributing to damage. Inhibiting them actually may cause further problems. We’re gearing up to do a set of studies that look at how certain immune cells, known as monocytes, respond to infection and how their response differs using a combination of Down syndrome models.
Journal information:
iScience
Source: Read Full Article