Thousands of Pacific Islanders who went years without promised Medicaid coverage before Congress made amends during the pandemic could lose those benefits this spring in the first wave of eligibility redeterminations.
Why it matters: States are culling their Medicaid rolls with the end of the COVID-19 emergency, removing guarantees of continuous coverage that reduced health inequities in ways obvious and not-so-obvious.
Zoom in: Consider the 94,000 individuals from the Marshall Islands, Palau and the Federated States of Micronesia now living in the U.S. While non-citizens, they're guaranteed Medicaid and CHIP benefits under a Reagan-era agreement that gave the U.S. exclusive use and control of sites in those islands for military activity.
- Congress erroneously stripped the group's Medicaid benefits when drafting welfare reform legislation in 1996. That left communities exposed to the ravages of COVID-19 more than other groups before Congress restored the benefits in a year-end spending package in 2020.
- Now, some of those same individuals could be forced out of the safety net program as states redetermine eligibility requirements.
- They include the Marshallese from islands that were the site of Cold War U.S. nuclear tests that left residents suffering from cancers, birth defects and forced relocations.
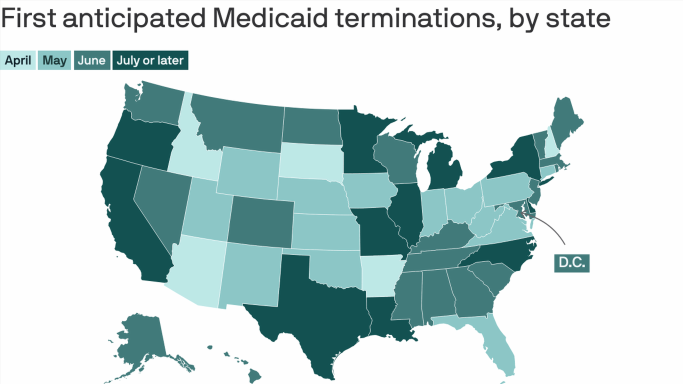
Arkansas, one of the largest Marshallese enclaves, started Medicaid redeterminations this month and will evaluate eligibility for upwards of 400,000 residents this year.
- An estimated 15,000 Marshallese lived in the state as of 2020, many drawn to the region's food processing plants for work or joining family on the mainland.
- After their Medicaid coverage was restored, upwards of 4,000 Pacific Islanders and Native Hawaiians living in Northwest Arkansas got health coverage from 2020 to 2022.
- The concern is for individuals who still may qualify for benefits but could be disenrolled and lost in the administrative churn due to language barriers, erroneous contact information or other factors.
State of play: Notices started going out earlier this year in Arkansas asking recipients to update their contact information, the first step of the redetermination process, and Michelle Pedro, community health worker and policy director at the Arkansas Coalition for the Marshallese, said her office has been flooded with questions.
- "We're doing a little bit more outreach than we anticipated," Pedro told Axios.
- The Medicaid benefits have been a lifeline for those residents, including in Northwest Arkansas, said Rep. Steve Womack (R-Ark.).
The bottom line: After 25 years without Medicaid benefits, some Pacific Islanders could fall through the cracks again unless states and health groups come up with workarounds, new processes and outreach.
This story is a part of a reporting fellowship sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund.
Source: Read Full Article