Scientists have known for decades that pregnancy requires a mother’s body to adjust so that her immune system does not attack the growing fetus as if it were a hostile foreign invader. Yet despite learning a great deal more about the immunology of pregnancy in recent years, a new study shows that the cellular cross-talk between a mother and her offspring is even more complex and long-lasting than expected.
The study was published online in the journal Science by a research team led by Sing Sing Way, MD, Ph.D., Division of Infectious Diseases at Cincinnati Children’s and the Center for Inflammation and Tolerance.
“By investigating how prior pregnancy changes the outcomes of future pregnancies—or in other words how mothers remember their babies—our findings add a new dimension to our understanding of how pregnancy works,” Way says.
“Nature has designed built-in resiliency in mothers that generally reduces the risk of preterm birth, preeclampsia, and stillbirth in women who have a prior healthy pregnancy. If we can learn ways to mimic these strategies, we may be better able to prevent complications in high-risk pregnancies.”
In addition to potentially making progress against the leading cause of infant mortality, Way says understanding how the immune system changes during pregnancy could influence other research fields including vaccine development, autoimmunity research, and how to prevent organ transplant rejection.
How moms remember their babies
In 2012, Way and colleagues published a study in Nature that revealed how the experience of a first pregnancy makes a woman’s body much less likely to reject a second pregnancy with the same father.
In addition to previously known short-term immune system adjustments, the researchers found that the mother’s body keeps a longer-term supply of immune suppressive T cells that specifically recognize the next fetus by the same couple. These suppressive T cells instruct the rest of the immune system to stand down as the pregnancy develops and linger in the mother’s body for years after giving birth.
For immunity against infection, such “memory” cells often require a constant, low level of exposure to the invading pathogen. So, initially, scientists were surprised to find these suppressive cells persisting in mothers well beyond childbirth.
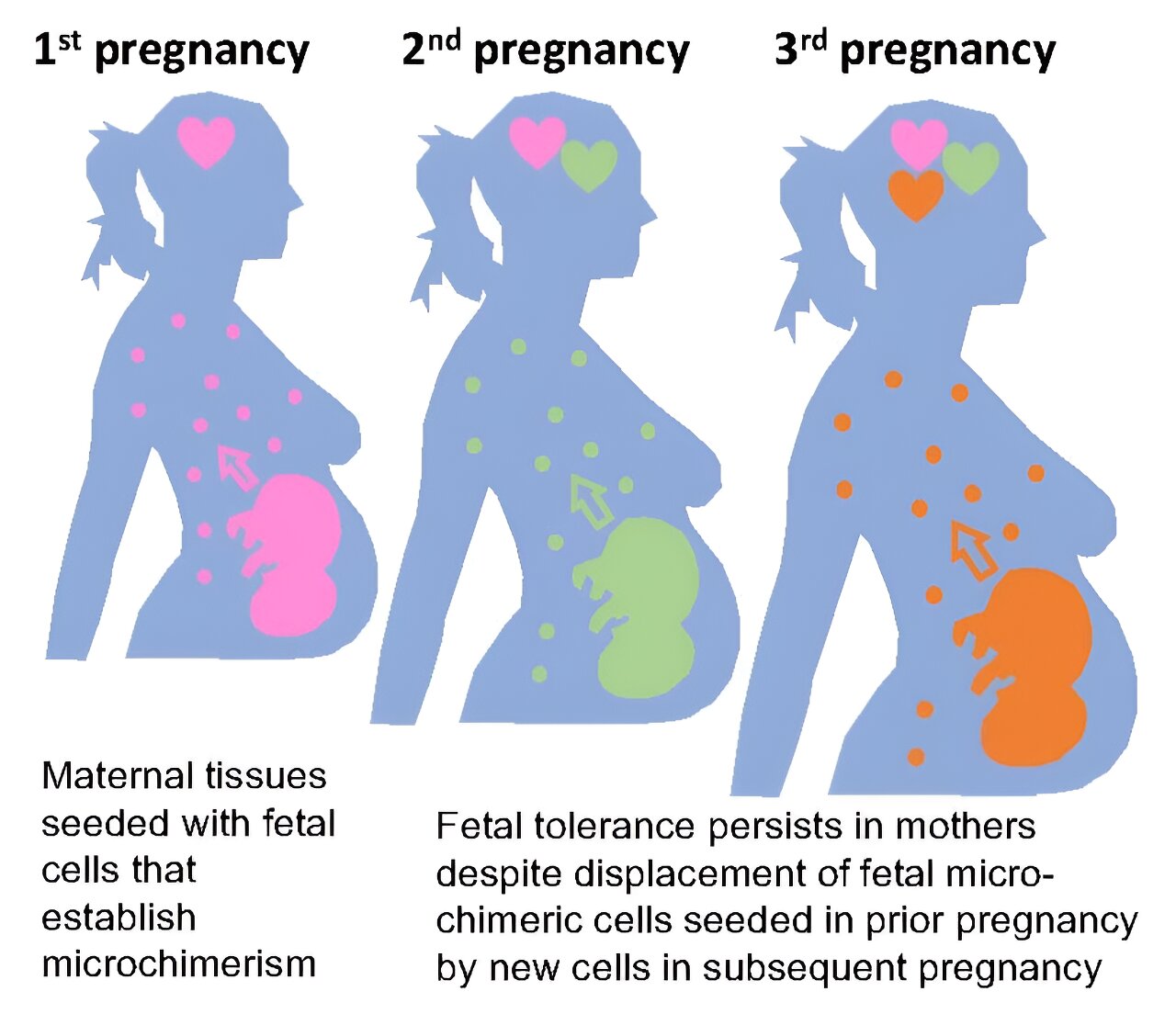
The new study in Science reports that maintaining protective memory suppressive T cells is mediated by tiny populations of baby cells that remain in mothers after pregnancy called fetal microchimeric cells. This finding provides further biological evidence to support a widely recognized special connection between mothers and their children.
“Very small numbers of fetal cells can be found in the heart, liver, intestine, uterus and other tissues,” Way says. “The fact that we are made up of more than just cells with our own genetics, but also cells from our mothers and our children is a fascinating idea.”
This influence linked to fetal cells builds on research Way and colleagues published in Cell in 2015 that shows children maintain a small supply of cells transferred from their mothers during pregnancy called maternal microchimeric cells. Even many years later, these cells help explain why an organ transplant from a person’s mother is more likely to be successful compared to a donor organ from their father.
But there’s more to the story, Way says.
This potentially wide assortment of genetically foreign cells in women, including maternal microchimeric cells from their mother and unique fetal microchimeric cells from each pregnancy raises fundamental new questions about how microchimeric cells interact with each other, and the limits of their accumulation. The current Science paper shows that each individual can have only one set of microchimeric cells at a time.
Fetal microchimeric cells remaining in mothers from a first pregnancy get displaced by new fetal cells when mothers become pregnant again. Meanwhile, once a grown daughter becomes pregnant, fetal microchimeric cells displace maternal microchimeric cells causing her to immunologically “forget” her mother.
“This transience for individual sets of microchimeric cells is remarkable, especially considering their protective benefits on pregnancy outcomes, and they represent only one in a million cells,” Way says.
However, the new research also shows that mothers never fully forget their children in the same way daughters forget their mothers. While the supply of protective fetal microchimeric cells reflect only the most recent pregnancy, a small number of suppressive T cells from each pregnancy lives on in a latent form within the mother. They can linger for years, until called into action by a new pregnancy.
“This was an unexpected finding,” Way says. “These memory immune cells with latent suppressive properties act as a fail-safe mechanism in addition to the protection from traditional memory suppressive T cells.”
Implications for high-risk pregnancy
While the new study is based on studying mouse models, the co-authors say a body of research already exists demonstrating the cellular crosstalk observed in the mice also happens in humans.
One emerging theory that requires further study is that a woman’s immune system may also “remember” bad pregnancy outcomes in much the same way it remembers good outcomes.
“The challenge will be to identify specifically what a mother’s immune system retains from a pregnancy with a poor outcome,” Way says. “If we can isolate how those mechanisms differ from a healthy outcome then we would have a target for developing improved treatments to improve outcomes in high-risk pregnancies.”
Way says it will likely take several years to translate the new study’s findings into possible treatments that could be tested in clinical trials.
Implications for vaccine research
While recommended for years by some experts, awareness has grown in recent years that providing vaccines to pregnant woman can protect their newborns from infectious disease threats long before the babies can directly receive their own vaccines.
In June 2022, Way and colleagues detailed in Nature how mothers can produce “super antibodies” that can protect newborns from infectious threats more effectively than previously thought possible. Their findings add weight to recommendations that pregnant women receive all the vaccines available to them.
In August 2023, that list of vaccines grew when the US Food and Drug Administration approved the first vaccine that can be given to pregnant women to protect newborns from RSV—the number one cause of lower respiratory tract illness in infants and toddlers. Around the world, some 45,000 children die each year from RSV, including about 300 children a year in the U.S. Another 80,000 babies a year in the U.S. get so sick from RSV that they require hospital care.
With new understanding emerging about how the immune system functions during pregnancy, Way predicts that even more vaccines will come along to protect both mother and child.
“We are just beginning to understand how mothers immunologically tolerate their babies during pregnancy. Considering parity or the outcomes of prior pregnancy on the outcomes of future pregnancies add an exciting new dimension for investigating how pregnancy works,” Way says.
“On the other hand, given the importance of reproductive fitness in trait selection, immunology learned from mothers and babies can open up new ways to improve vaccines, autoimmunity and transplantation.”
More information:
Tzu-Yu Shao et al, Reproductive outcomes after pregnancy-induced displacement of preexisting microchimeric cells, Science (2023). DOI: 10.1126/science.adf9325. www.science.org/doi/10.1126/science.adf9325
Journal information:
Nature
,
Science
,
Cell
Source: Read Full Article