In a recent study posted to the medRxiv* preprint server, researchers examined the coronavirus disease 2019 (COVID-19) vaccine uptake and hesitancy among people with chronic or severe health conditions.
Studies reported that one in every three individuals aged 16 years or above has a chronic condition. These medically vulnerable people are at an elevated risk of COVID-19-related severe complications and death. The most effective defense against the COVID-19 pandemic has been vaccines against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Since its advent, COVID-19 vaccination has significantly impacted public health. Health care workers and vulnerable populations were first prioritized, and gradually, the vaccination program was expanded to cover different population groups.
Nonetheless, several countries faced challenges in vaccinating people, and vaccine hesitancy grew significantly, including among the susceptible population. In 2019, the World Health Organization (WHO) classified vaccine hesitancy as one of the top threats to public health. As with SARS-CoV-2 vaccination, reports have suggested that up to half of the general population is skeptical about vaccination with regional variability.
 Study: Serious underlying medical conditions and COVID-19 vaccine hesitancy. Image Credit: FrankHH / Shutterstock
Study: Serious underlying medical conditions and COVID-19 vaccine hesitancy. Image Credit: FrankHH / Shutterstock
About the study
In the present study, researchers evaluated SARS-CoV-2 vaccine intent, uptake, and hesitancy to understand the general and disease-associated beliefs among individuals with diabetes, cancer, and multiple sclerosis (MS).
The study was conducted in four Australian states with a 4.9 million catchment population. The survey commenced on June 30, 2021, and ended on October 5, 2021, a period that witnessed varying lockdowns and rollout of vaccines.
Eligible participants were aged 18 years or higher and had either past or current diagnoses of MS, diabetes, or solid organ/hematological malignancy. Demographic factors such as age, education, gender, household income range, and clinical parameters like time since diagnosis and current treatment were surveyed.
The Oxford COVID-19 vaccine hesitancy scale, a measure of vaccine uptake willingness, was adapted with minor modifications in which a higher score was indicative of greater hesitancy. Of the 14-item Oxford COVID-19 vaccine confidence and complacency scale, 11 items were adapted for the present study, with higher scores reflecting a negative vaccination attitude. A disease-influenced vaccine acceptance scale 6 (DIVAS-6) evaluated vaccine-related views originating from concerns regarding underlying conditions and treatment of patients.
Demographic and individual scale item differences were evaluated through chi-square tests and independent sample t-tests. Logistic regression analysis determined if the scales could predict vaccination status, and linear regression analysis was performed to assess if the Oxford scales' total and subscale scores could predict vaccine acceptance.
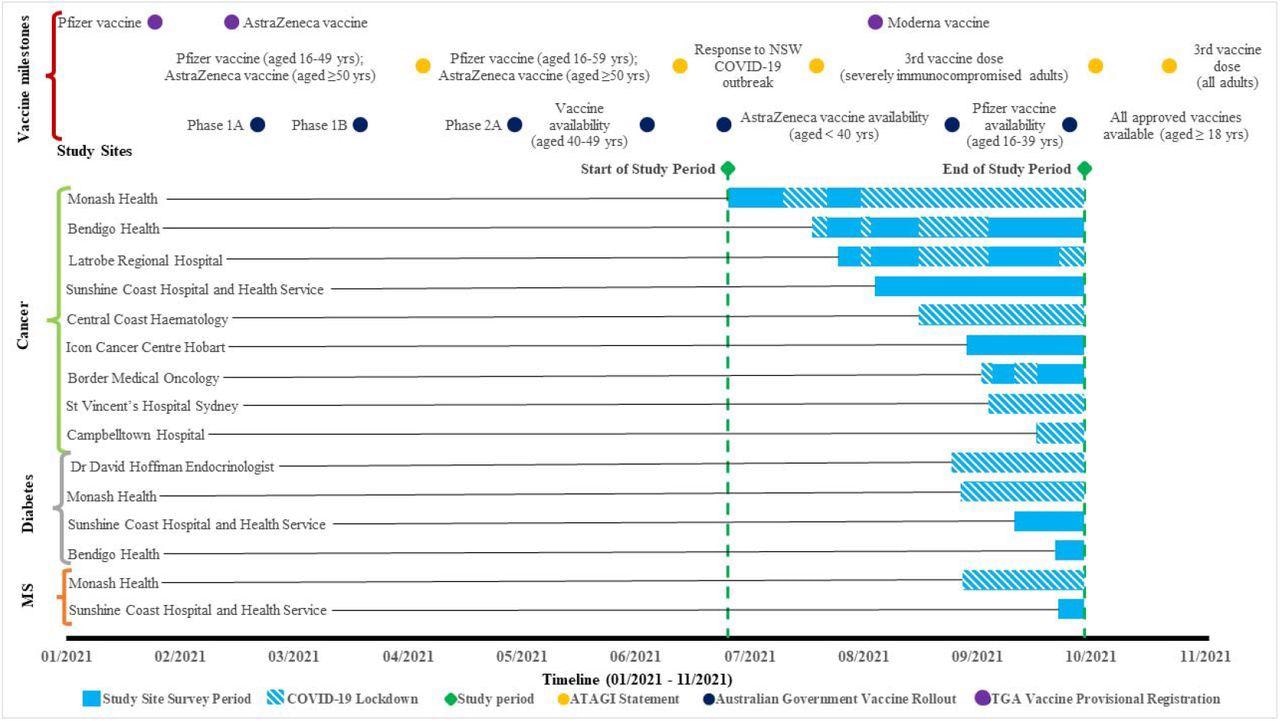
Survey timeline for each health service and participant group, with Australian State Government COVID-19 lockdowns embedded in the study site survey period. Yrs = years; MS = multiple sclerosis; ATAGI = Australian Technical Advisory Group on Immunisation; TGA = Therapeutic Goods Administration. Australian Government Vaccine Rollout Phase population group eligibility: Phase 1A rollout = Quarantine and border workers, health care workers, aged and disability residents and staff; Phase 1B rollout = Adults aged 70 years and over, Aboriginal and Torres Strait Islander people aged 55 years and over, Adults with underlying medical conditions, other critical and high-risk workers; Phase 2A rollout = Adults aged 50 years and over, Aboriginal and Torres Strait Islander people aged 18 years and over.
Findings
4,683 responses were analyzed after removing duplicate, incomplete or ineligible responses. Of these, 3,560 responses were from cancer patients, 842 from diabetic people, and 281 from MS patients. Breast cancer (27.7%) was the most common type, and more than half of the cancer patients were currently receiving treatment. Type 2 diabetes was most common (66.2%) among diabetic patients, and more than 98% of them were currently receiving treatments.
Over 81% of the participants had received at least one SARS-CoV-2 vaccine, similar to the national average. No statistically significant differences were found in vaccine uptake among the disease types. Around 90% of participants mentioned that they had or would accept the SARS-CoV-2 vaccine, 5.8% said they were unsure, and 4.3% were hesitant. About 52% of non-vaccinated participants expressed willingness to be vaccinated, and 22.7% expressed hesitancy. The non-vaccinated subjects scored significantly higher on the Oxford hesitancy scale regardless of disease type.
Similarly, non-vaccinated respondents had higher scores on the confidence and complacency scale, highlighting a negative attitude towards COVID-19 vaccination. Overall, 60.6% of participants were worried about SARS-CoV-2 infection, and 69.9% of respondents felt that vaccination was necessary due to the presence of underlying medical conditions.
Many participants (44%) had concerns about the efficacy of vaccines due to the underlying condition, while 39.6% (or 25.7%) raised concerns over the effect of vaccines on their disease (or treatment). Non-vaccinated subjects scored higher on the DIVAS-6 total and subscale scores, reflecting higher complacency for SARS-CoV-2 infection, concerns over vaccine efficacy, and the effect of vaccines on their health condition or treatment.
Conclusions
The authors observed that the underlying health conditions significantly influenced the uptake and attitude towards COVID-19 vaccines. The type and degree of concerns were shared across the three disease groups. Given the intrinsic vulnerability, vaccination hesitancy was lower in the studied cohorts than in the general population. Overall, the study population exhibited a high vaccination rate and expressed positive intent to vaccinate, which was influenced by their concerns about the impact of COVID-19 on their underlying medical conditions.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Serious underlying medical conditions and COVID-19 vaccine hesitancy.Daphne Day, Lisa Grech, Mike Nguyen, Nathan Bain, Alastair Kwok, Sam Harris, Hieu Chau, Bryan Chan, Richard Blennerhassett, Louise Nott, Nada Hamad, Annette Tognela, David Hoffman, Amelia McCartney, Kate Webber, Jennifer Wong, Craig Underhill, Brett Sillars, Antony Winkel, Mark Savage, Bao Sheng Loe, Daniel Freeman, Eva Segelov, medRxiv preprint 2022, DOI: https://doi.org/10.1101/2022.04.06.22273080, https://www.medrxiv.org/content/10.1101/2022.04.06.22273080v1
Posted in: Men's Health News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Breast Cancer, Cancer, Chronic, Coronavirus, Coronavirus Disease COVID-19, Diabetes, Disability, Education, Efficacy, Health Care, Multiple Sclerosis, Pandemic, Public Health, Respiratory, SARS, SARS-CoV-2, Sclerosis, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Type 2 Diabetes, Vaccine

Written by
Tarun Sai Lomte
Tarun is a writer based in Hyderabad, India. He has a Master’s degree in Biotechnology from the University of Hyderabad and is enthusiastic about scientific research. He enjoys reading research papers and literature reviews and is passionate about writing.
Source: Read Full Article