A lung transplant can mean the difference between life and death for people with diseases such as pulmonary fibrosis, chronic obstructive pulmonary disease (COPD) and even severe COVID-19. Yet, recipients of donor lungs must take daily medications to stave off damage caused by their own immune system, which attacks the organs it recognizes as foreign—a process known as rejection.
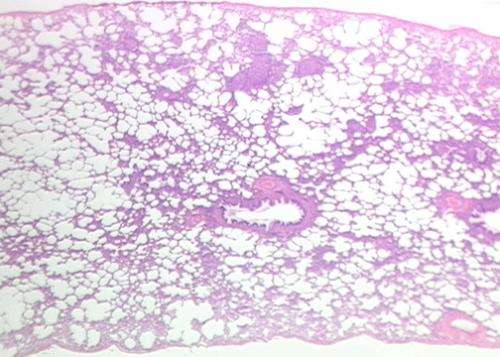
A new University of Michigan Health study, published in the Journal of Clinical Investigation, has identified cells that appear to play a pivotal role in creating the scarring, or fibrosis, characteristic of chronic rejection following a lung transplant.
Almost 15 years ago, Vibha Lama, MBBS, M.S., a professor in the Division of Pulmonary Disease and Critical Care Medicine, and her lab described the presence of stem-cell-like cells, called mesenchymal stromal cells, in lung sample fluid from lung transplant recipients.
“We found that even ten years post-transplant, these cells belonged to the donor, not the recipient,” she explained. “At that time, we had no clue where in the lung they were coming from or what role they played.”
To figure this out, her lab generated a mouse model to recreate what happens within a lung transplant recipient. With the model, they followed a transcription factor known as FOXF1 as a sort of trail of breadcrumbs back to the cells’ original location.
They discovered that these cells formed a reservoir of stem cells within the bronchovascular bundle deep inside the lung. These bundles contain a bronchus (airway), arteries, connective tissue and other structures and is the part of the lung which connects it to the outside environment.
In this study, explained Lama, who is senior author on the paper, they show that these specific stem cells are interacting with neighboring epithelial cells within that airway niche.
Epithelial cells line and protect the airways and produce a protein known as Sonic hedgehog. Via this protein, epithelial cells signal the stem-cell-like mesenchymal cells, which make up the scaffolding of the lungs, to make FOXF1, a repressor that keeps the stem cells in check.
“We are just recently understanding that there are many different kinds of mesenchymal cells in the lung,” said Lama. “What we describe here is not only are there many kinds of mesenchymal cells, FOXF1 is retained only in these specific stem-cell-like cells.”
In the case of lung transplant rejection, Lama hypothesized that immune cells from the recipient attack the epithelial cells which disrupts the balance between them and the mesenchymal cells.
“Because of the damage caused by rejection, the epithelial cells get damaged, Sonic hedgehog is reduced and that interrupts the signaling to the mesenchymal cells to keep quiet,” she said. “Because of that, these cells start dividing and they lay down more collagen, which leads to fibrotic scarring.”
Source: Read Full Article
