Researchers at UC Santa Cruz have developed a novel serological assay for the detection of antibodies to SARS-CoV-2, the coronavirus that causes COVID-19.
Rebecca DuBois, associate professor of biomolecular engineering at UC Santa Cruz, said the new method her team developed is as accurate as the most reliable antibody tests currently available, but is less complex and can be performed much faster.
The gold standard for serological testing is a complex laboratory method called ELISA that takes four to six hours to run and provides quantitative results indicating the strength of the immune response. Simpler assays using test strips provide rapid results, but are less reliable and do not quantify antibody levels.
The new method, called biolayer interferometry immunosorbent assay (BLI-ISA), provides complete quantitative results in less than 20 minutes. DuBois and her colleagues described the assay in a paper published December 10 in Scientific Reports.
“Our assay is as sensitive if not better than other assays in detecting low levels of antibodies, and the specificity [false-positive rate] is as good as the best antibody tests out there,” DuBois said. “It combines the advantages of the test strips that take 20 minutes with the quantitative results and higher performance of ELISA.”
A positive antibody test indicates prior infection with the virus. These tests are not used to diagnose active infections, however, which requires a different test that detects the virus’s genetic material or the virus antigens. Antibodies are proteins made by the immune system that recognize and bind to virus antigens.
Serological testing is important for understanding the spread of the coronavirus by determining how many people in a population have been infected. The tests are also used to evaluate the responses to experimental vaccines in both people and laboratory animals. Quantitative information about antibody levels could be especially important in the future if scientists are able to determine that a certain level of particular antibodies is needed to provide protection against infection with the coronavirus.
“That is still to be determined, but we do know that people who have been infected with SARS-CoV-2 have very diverse levels of antibodies, and it would not be surprising to find that below some baseline level they might not be protective,” DuBois said. “So it’s really useful to have that quantitative ability to know what someone’s antibody status is, whether it’s from a past infection or a vaccination.”

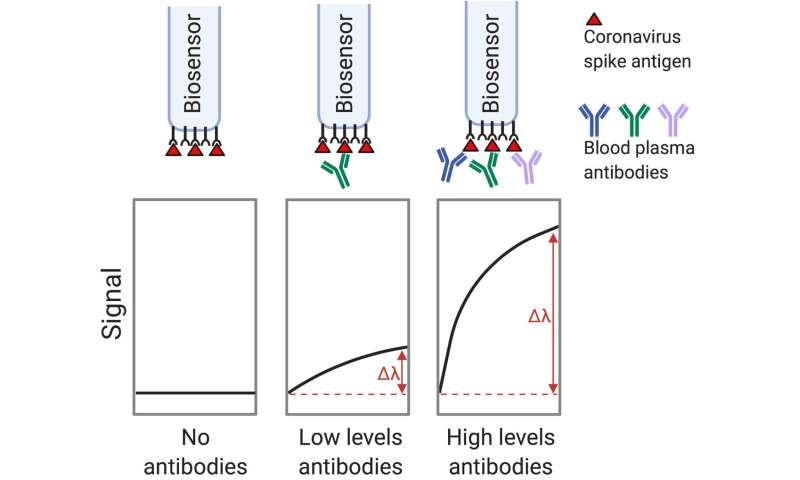
The new BLI-ISA method uses biolayer interferometry, an optical technique for measuring the interactions between molecules by detecting the binding of molecules to the tip of a fiber-optic biosensor. The instruments required to perform biolayer interferometry are increasingly common in research laboratories. The BLI instrument at UCSC is used by several research groups, and DuBois has been using it in her research to study antibody-antigen interactions.
The new serological assay involves several steps performed by the instrument in an automated “dip-and-read” format. In the first step, the biosensor tip is dipped into a solution containing the antigen (a viral protein) that is recognized by the antibody to be tested for. As the antigen binds to the biosensor tip, it generates a signal that can be used for quality control to ensure consistency in the antigen loading step. Next, after dipping into a wash solution, the biosensor is dipped into the blood plasma sample, generating a signal as antibodies bind to the antigen.
The immune system makes different types of antibodies, called isotypes, including IgM, which is produced early in the infection and declines later, and IgG, which is produced later and persists longer. In the antibody binding step, the BLI instrument detects any type of antibody that binds to the antigen.
“Depending on when the blood sample was taken after infection, there might be different types of antibodies, and this step gives us the total antibody level,” DuBois said.
The next step detects and quantifies IgG antibodies specifically by measuring the binding of anti-IgG antibodies. The assay thereby provides quantitative measurements of both total antibodies and IgG antibodies, and it can be designed to measure different isotypes as well.
In response to infection with the coronavirus, the immune system makes antibodies against a range of different coronavirus antigens. Most serological testing methods for SARS-CoV-2 are designed to detect antibodies to structural proteins of the virus such as the spike protein, which studs the surface of the virus and enables it to bind to and enter human cells. Antibodies to one part of the spike protein—the receptor binding domain, or RBD—are of particular interest because they are effective at neutralizing the virus in laboratory assays.
DuBois’s team developed and tested the new assay using RBD antigens, but she noted that it can be used to detect a wide range of antigens. The BLI instrument allows easy “multiplexing,” meaning that multiple tests can be run in parallel on the same blood sample to detect antibodies to different viral antigens as well as different antibody isotypes.
Because it requires laboratory equipment, BLI-ISA could not be used as a point-of-care test at doctor’s offices or pharmacies. But it allows high-throughput processing of samples and is faster and less labor intensive than other quantitative laboratory tests such as ELISA, Immunofluorescent Assay, and Chemiluminescent Immunoassay. The amount of blood needed for the test can be obtained with a finger prick.
Another advantage of BLI-ISA over other methods is the ease of standardizing the assay so that a sample gives the same quantitative results in repeated tests at different times or in different laboratories. ELISA requires an enzyme-based signal amplification step, which can vary depending on temperature and other factors, resulting in much more test-to-test variability in the quantitative measurements.
First author John Dzimianski, a postdoctoral researcher in DuBois’s lab, said the new assay could be especially useful for researchers in vaccine development. “This method provides a standardized way to quantify antibody levels, which could be used to compare antibody responses to different vaccine candidates. In addition, running the assay itself is straightforward, requiring little more than the push of a button,” he said. “It’s a simple but powerful tool.”
Source: Read Full Article
