Since severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged, multiple variants of concern (VOCs) have arisen. These variants of concern show enhanced infectivity, immune evasion, and many vaccines have lower effectivity against them. As governments begin to dismantle pandemic safety measures such as lockdowns, social distancing, and mandatory face masks, coronavirus disease 2019 (COVID-19) cases are on the rise, many of which are caused by variants.
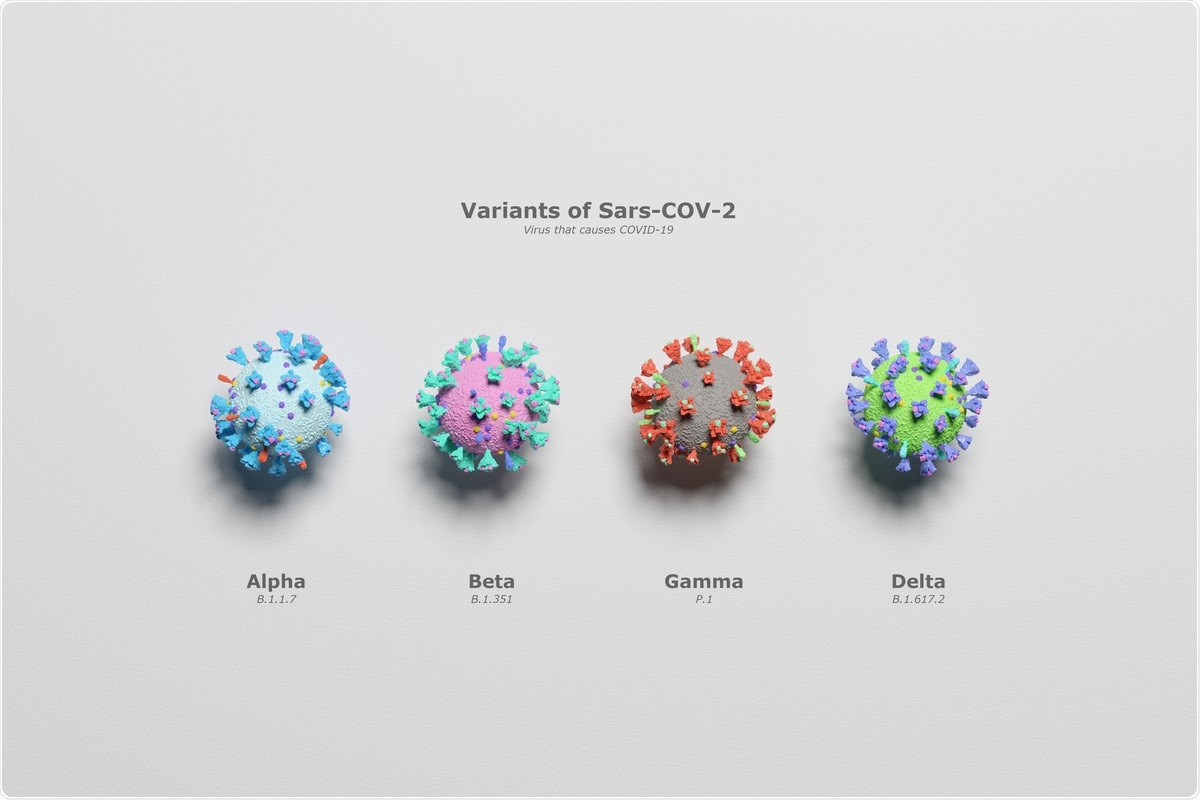 Study: Molecular insights into receptor binding of recent emerging SARS-CoV-2 variants. Image Credit: Mediantone/ Shutterstock
Study: Molecular insights into receptor binding of recent emerging SARS-CoV-2 variants. Image Credit: Mediantone/ Shutterstock
Of particular concern is the Delta variant, which shows increased transmission and can evade both vaccine-induced and natural immunity – and now accounts for over 90% of new cases. There have even been cases of the virus spreading from humans into animals. In a study published in Nature Communications, researchers from the Chinese Academy Of Sciences have been investigating the changes in receptor binding in these variants that increase the danger they pose.
Background
Many vaccines and monoclonal antibodies target the spike protein of SARS-CoV-2. It is key to the pathogenicity of COVID-19. It consists of two subunits – S1, which contains a receptor-binding domain (RBD) that primarily binds to angiotensin-converting enzyme 2 (ACE2) to allow viral cell entry, and S2, which is primarily responsible for membrane fusion. The spike protein is a trimer and many of the mutations that variants carry affect the conformation of this trimer.
The monomers that form it can present in two positions – up and down. In wild-type, the monomers primarily show a conformation of all-down or one-up two-down. This reduces the probability of provoking an immune reaction. However, in variants, more of the monomers normally show as up, increasing ACE2 binding and infectivity.
The study
The researchers examined the binding of six SARS-CoV-2 variants to human ACE2, including Alpha, Beta, and Gamma, as well as three strains found in Mink – Mink-Y453F, Mink-F486L and Mink-501T. These were then compared to wild-type SARS-CoV-2 binding. The RBDs of the variants and wild—type were purified and evaluated for ACE2 binding using flow cytometry. All of the variants commonly found in humans showed increased binding to ACE2 compared to wild-type and two of the Mink variants.
Further investigating these interactions, the binding affinity of these RBDs was assessed using surface plasmon resonance (SPR), a technique in which the oscillation of electrons at the interface between negative and positive permittivity material is stimulated by light, allowing the adsorption of materials to be measured. Mouse Fc (mFc) tagged ACE2 was immobilized with an anti-mFC antibody in a chip, and the variants flowed through this. Mink-N501T showed the highest affinity compared to wild type, with an 8-fold increase in binding ability. Alpha, Beta, Gamma, and Mink Y453F RBD all showed higher affinity than wild-type, with 7, 3, 5, and 4-fold increases in binding ability, respectively.
Next, the researchers examined which mutations within Alpha, Beta, and Gamma contributed to the differing affinities. Alpha contains fewer mutations than the other two variants but shows a higher affinity, so some mutations must result in residues that lower the affinity. The researchers generated single and double mutated RBD and examined the binding affinity for ACE2. Two mutations, K417N and K417T showed reduced affinity, as did double mutations. E484K showed little effect.
To investigate the underlying mechanisms of the differences in binding ability, the researchers created crystal structures at various resolutions of variants RBDs bound to ACE2. Each structure is compromised of one copy of the complex molecule in one unit.
They showed that N501 is located in a loop structure in all human variants and cannot be replaced by a Y. Only weak hydrogen bonds can form between N501 and ACE2. However, a phenyl on the Y501 side chain shows many sites that could interact with ACE2. These results are supported by previous studies identifying the structure of N501. The reason for the lower binding affinity in Gamma and Beta compared to Alpha can be traced back to the K417N and K417T mutations, which destroy the salt bridge formed by K417 and an ACE2 residue.
Conclusion
The researchers highlight the importance of their study in helping to characterize ACE2 binding, which should provide further information into the comparative transduction efficiency of the SARS-CoV-2 variants. This helps understand the transmission of the disease and inform public health policymakers, epidemiologists, and those modeling the spread and evolution of the disease. This information could help determine methods to prevent new variants of the disease from forcing many governments into costly new restrictions – changes that would likely reignite the economic crises of the early days of the pandemic.
- Han, P. et al., (2021) Molecular insights into receptor binding of recent emerging SARS-CoV-2 variants. Nature Communications. doi: https://doi.org/10.1038/s41467-021-26401-w
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, binding affinity, Cell, CHIP, Coronavirus, Coronavirus Disease COVID-19, Cytometry, Enzyme, Evolution, Flow Cytometry, immunity, Membrane, Molecule, Pandemic, Protein, Public Health, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus

Written by
Sam Hancock
Sam completed his MSci in Genetics at the University of Nottingham in 2019, fuelled initially by an interest in genetic ageing. As part of his degree, he also investigated the role of rnh genes in originless replication in archaea.
Source: Read Full Article
