Extremely low rates of testing of bone mineral density (BMD), as recommended by recent guidelines, were found in a nationwide study of older men receiving androgen deprivation therapy (ADT) for the treatment of prostate cancer.
Even fewer men with Medicare Part D coverage who were at risk for fracture were being treated with a bone-modifying agent.
“Androgen deprivation therapy (ADT) is the mainstay for treatment of locally advanced high-risk localized or metastatic prostate cancer [but it] can negatively impact bone health, resulting in decreased bone mineral density (BMD) and fractures,” comment the researchers, led by Maria Suarez-Almazor, MD, PhD, University of Texas MD Anderson Cancer Center, Houston, Texas.
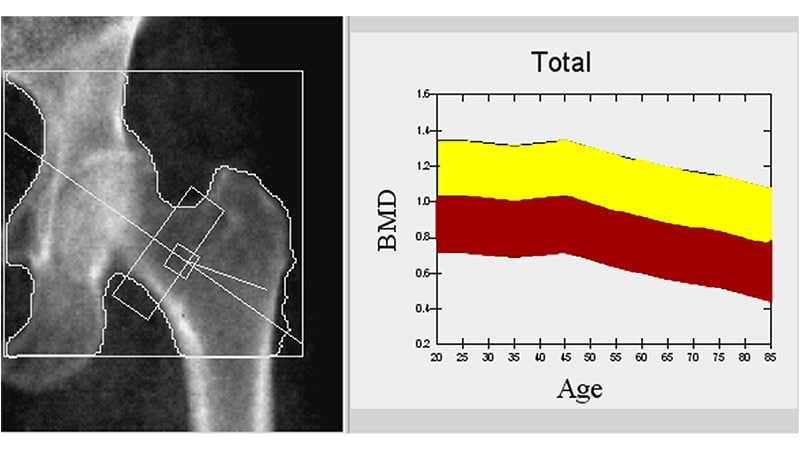
Although they found low rates of screening of BMD with a DXA (dual-energy x-ray absorptiomentry) scans, use of such a scan “was associated with a lower risk of major fractures,” they write.
This suggests that “DXA screening is important for the prevention of major fractures among older men with prostate cancer,” they conclude.
The study was published online April 1 in JAMA Network Open.
Fracture Risk
For their study, the team used data from the Surveillance, Epidemiology, and End Results database as well as the Texas Cancer Registry.
They identified 54,953 men (median age, 74 years) who had been diagnosed with localized or regional prostate cancer between January 2005 and December 2015.
Overall, only 7.9% of men had undergone DXA screening, although screening rates increased from 6.8% in 2005 to 8.4% in 2015.
Overall, 17.5% of men experienced a fracture after initial receipt of ADT; the median time to first fracture was 31 months. Some 7.7% of men experienced a major osteoporotic fracture.
While DXA screening was not associated with fracture risk at any site, it was associated with a 9.1% lower risk of a major osteoporotic fracture, the authors note.
Some of the lowest rates of DXA screening were seen among Black men as well as single men and those who had a full or partial state insurance buy-in, which is a proxy of socioeconomic status, the authors observe.
Higher rates of DXA screening were seen in men who had recently begun ADT, those who were older, those who had regional or high-grade disease, those who had previously had a fracture, those with known osteoporosis, and/or those with a higher Charlson comorbidity score.
Professional Society Guidelines Updated
The study ended in 2015; since then, nearly all professional society guidelines have been updated regarding the need for DXA screening, point out the authors of an accompanying editorial.
“Thus, DNA screening rates in more recent years may be higher,” suggest the editorialists, led by Amar Kishan, MD, University of California, Los Angeles.
In addition, they suggest that the fractures observed in this study “may be associated with skeletal metastases rather than osteopenia or osteoporosis that was not appropriately managed,” because over 70% of patients in this study had high-grade disease. Given that the median time to fracture was 31 months in the current study, “these fractures may have reflected progression events,” they observe.
At the same time, this study highlights the fact that there is substantial room for improvement in evaluating men who receive ADT for bone health, the editorialists comment. “It is particularly problematic that low rates of DXA screening were identified among men who were non-Hispanic Black, single, or residing in areas with lower socioeconomic status and lower education levels,” they say.
The solution could be quite straightforward. However modest the association between DXA screening and major fracture risk was, “it is possible that a simple intervention, such as supplemental vitamin D and calcium, could optimize bone health,” the editorialists comment.
“An increased rate of DXA screening among men receiving long-term ADT, along with appropriate use of bone-modifying agents…may meaningfully reduce the chance of osteoporosis-related fractures,” they conclude.
The study was funded by the Texas Department of State Health Services and the CPRIT. Suarez-Almazor reports receiving consulting fees from Avenue Therapeutics, Celgene, ChemoCentryx, Eli Lilly and Company, Gilead Sciences, and Pfizer. Kishan reports receiving grants from the American Society for Radiation Oncology, the National Institutes of Health, the Prostate Cancer Foundation, the US Department of Defense, and ViewRay, as well as honoraria and consulting fees from Varian Medical System and ViewRay. He also owns shares in ViewRay.
JAMA Netw Open. Published online April 1, 2022. Full text, Editorial
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article