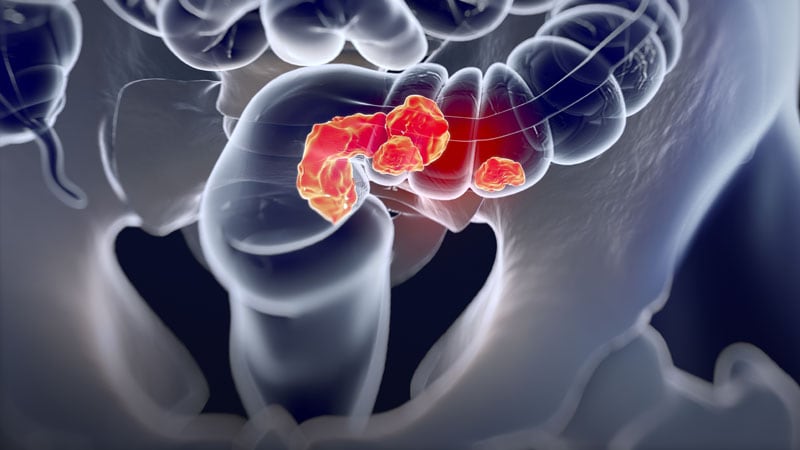
Patients with locally advanced rectal cancer and tumors with deficient mismatch repair (dMMR) have shown a remarkable response to treatment with the programmed cell death-1 (PD-1) inhibitor dostarlimab (Jemperli).
So far, the study has involved only 12 patients, but all of them have had a clinical complete response to treatment. They continue to show no signs of cancer (during follow-up ranging from 6 to 25 months) and have not undergone surgery or had radiation and chemotherapy, which are the standard treatment approaches.
The results were presented (abstract 16) at the American Society of Clinical Oncology 2022 annual meeting and simultaneously published June 5 in the New England Journal of Medicine.
“In our study, the elimination of tumors after 6 months of therapy with PD-1 blockade enabled us to omit both chemoradiotherapy and surgery and to proceed with observation alone,” say the authors, led by Andrea Cercek, MD, Memorial Sloan Kettering Cancer Center, New York City.
About 5%-10% of patients with rectal cancer have tumors with dMMR.
“The implications for quality of life are substantial, especially among patients in whom standard treatment would affect child-bearing potential [and] given that the incidence of rectal cancer is rising among young adults of childbearing age, the use of PD-1 blockade to eliminate the need for chemoradiotherapy and surgery may confer a particular benefit in that age group,” the authors comment.
The results of the current study are cause for “great optimism, but such an approach cannot yet supplant our current curative treatment approach,” comments Hanna Sanoff, MD, MPH, University of North Carolina Chapel Hill, writing in an accompanying editorial.
Single-Agent Dostarlimab
For the study, all patients were treated with single-agent dostarlimab every 3 weeks for 6 months.
Dostarlimab is already approved by the US Food and Drug Administration for use in the treatment of recurrent or advanced endometrial cancer with dMMR. Rectal cancer is an off-label use.
All patients had mismatch repair-deficient stage 2 or 3 rectal adenocarcinoma. The authors note that these tumors respond poorly to standard chemotherapy regimens, including neoadjuvant chemotherapy. The median age of enrolled patients was 54 years and 62% were women.
For the study, investigators planned that patients who had a clinical complete response after completion of dostarlimab were to proceed to observation without undergoing either chemoradiotherapy or surgery, while those who did not have a complete response were to have received these standard treatments.
As it turned out, all 12 patients achieved a complete response and have been followed by observation alone. The median follow-up from time of enrollment to data cutoff for the 12 patients was 12 months.
“Therapeutic responses were rapid,” the authors note, “with resolution of symptoms within 8 weeks after initiation of dostarlimab in 81% of the patients.”
To date, four patients have had 1 year of sustained clinical complete response after completion of the anti-PD-1 course.
In addition to the 12 patients documented in the study, another four patients have received at least one dose of dostarlimab and continue to receive treatment.
Adverse events occurred in most patients but none were grade 3 or higher. The most common grade 1 or 2 adverse events were rash or dermatitis, pruritus, fatigue, nausea and, in one patient, thyroid-function abnormalities.
The authors speculate that in addition to the extremely high tumor mutational burden associated with mismatch-repair deficiency, a tumor cell-extrinsic factor such as the gut microbiome may be driving the exceptionally good response to PD-1 blockade seen in this patient population.
Editorial Commentary
In the editorial, Sanoff emphasizes that the approach remains experimental and should not replace current curative treatment. She notes that cancer recurrences have been seen in other studies using both chemotherapy and immunotherapy.
For example, with chemotherapy and radiation, those patients who achieve a clinical complete response have a better prognosis than those who do not, but she cautions that “cancer regrowth occurs in 20% to 30% of such patients when the cancer is managed nonoperatively.”
Sanoff also notes that recurrences were seen when this approach of PD-1 inhibition has been used for metastatic colorectal cancer with dMMR. In the KEYNOTE-177 trial with pembrolizumab (Yervoy), only 55% of patients were reported to be alive without cancer progression at 12 months, and of the patients who initially had a strong response, only 70% had an ongoing response 3 years later.
“These recurrence dynamics may (or may not) differ between immunotherapy and chemoradiotherapy and between early and late-stage disease,” Sanoff comments.
“In fact, very little is known about the duration of time needed to find out whether a clinical complete response to dostarlimab equates to cure,” she adds.
In addition, Sanoff warns that the decision not to pursue further treatment, and follow patients with observation alone, requires very close monitoring.
The current study was conducted at a top US cancer center, the Memorial Sloan Kettering Cancer Center. The authors note that the complete responses (after a minimum of 6 months of follow-up) were measured by the combination of rectal MRI, visual endoscopic inspection, and digital rectal examination.
The completeness of these responses was further supported by the absence of residual tumor on serial endoscopic biopsies and the resolution of 18F-fluorodeoxyglucose uptake on PET scans, they add.
In the editorial, Sanoff comments that “safe nonoperative management [also] involves access to specialty care for direct intraluminal visualization and expertise in interpretation of rectal magnetic resonance imaging…Such expertise is not available in all communities and without it, patients could miss the opportunity for curative resection if tumor regrowth occurred.”
The study was sponsored by the Simon and Eve Colin Foundation, GlaxoSmithKline, and Stand Up to Cancer, among others.
N Engl J Med. Published online June 5, 2022. Full text, Editorial
Follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article