COVID-19 has changed life so significantly that it can sometimes be tough to remember what life was like without it. Social distancing, mask usage, and doing your best to stay home are all “normal” these days. You may be wondering as a result: When will the COVID-19 pandemic actually be over?
Experts swear this weird version of reality won’t last forever. Vaccines for COVID-19 have been authorized by the Food and Drug Administration (FDA) and are currently being distributed.
The short answer to that question is, no one can say for certain (sorry!). But infectious disease specialists and researchers have some thoughts to help put this global health situation into perspective.
How long will people be dealing with COVID-19 in the U.S. and around the world?
Honestly, it’s impossible to say if and when the coronavirus will die down because it’s still a new virus, and therefore unpredictable, says Faheem Younus, MD, the chief of infectious diseases at University of Maryland Upper Chesapeake Health. But pandemics have happened before, and they eventually pass as they become more contained, and as vaccines are developed and distributed. But researchers do look at past pandemics to make very baseline predictions about when it might end. In the past, pandemics have typically lasted between 12 and 36 months.
Sign up for WH Stronger for unlimited site access and more
Here’s one example of the timeline of a past pandemic: In 2009, a novel H1N1 flu pandemic occurred. (Remember swine flu?) The WHO declared a pandemic that June, and by mid-September, the FDA approved four vaccines for the virus, and they started getting administered in October. In late December, vaccination was opened up to anyone who wanted it, and the pandemic was deemed over in August 2010, according to a timeline from the CDC.
In the past, pandemics have typically lasted between 12 and 36 months.
The bummer is, though, you can’t simply model a new pandemic against a past one and accurately determine how bad or long *this* pandemic will be—because they are not the same viruses, and viruses behave and spread differently, says Rishi Desai, MD, a former epidemic intelligence service officer in the division of viral diseases at the CDC. But as more info becomes available about COVID-19, better predictions will be made. “My expectation is that COVID-19 will continue to be a threat for a good part of 2020, and that we will start to see the page turn in 2021,” Dr. Desai says.
Some good news is that vaccines are already being distributed to high priority groups and, with that, people should develop immunity to the virus. But even so, we could be doing this weird version of reality for a while, saysClyde Yancy, MD, vice dean for diversity and inclusion at Northwestern Medicine. “Every prediction that anyone might say would be a rough approximation—from me included,” he says.
Sounds like we’ve made serious progress on vaccines. What’s the update?
As of right now, the FDA has authorized two vaccines for use against COVID-19: One from Pfizer-BioNTech, and another from Moderna.
Both vaccines use a newish technology called messenger RNA (mRNA). These vaccines work by encoding a portion of the spike protein found on the surface of SARS-CoV-2, the virus that causes COVID-19, according to the Centers for Disease Control and Prevention (CDC). That creates an immune response in your body, causing it to develop antibodies, i.e. proteins created by your immune system to help it fight off particular infections. (In this case, the antibodies will target SARS-CoV-2 in the future.)
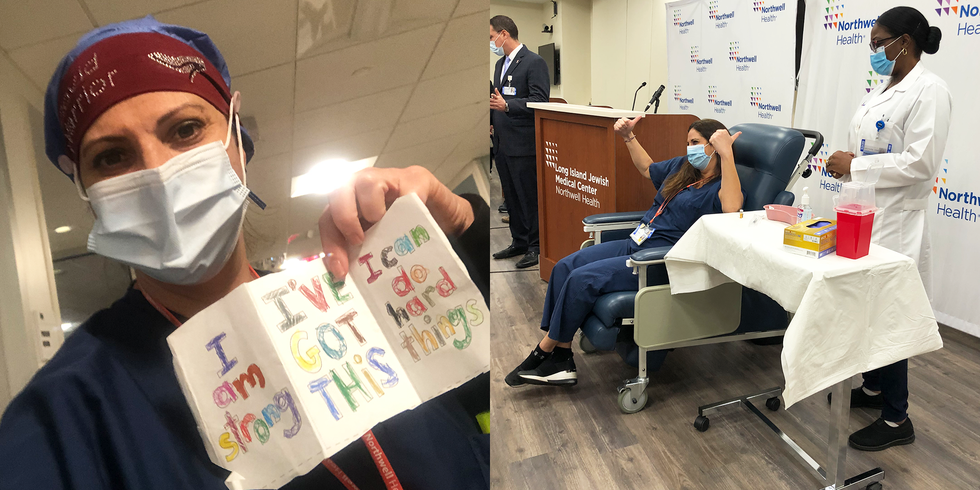
The vaccines are both highly effective. Pfizer’s is 90 percent effective at preventing future COVID-19 infections, while Moderna’s is 94.5 percent effective at preventing infections. “What’s unclear at this point, though, is whether they can prevent people from spreading the virus,” says John Sellick, DO, an infectious disease expert and professor of medicine at the University at Buffalo/SUNY in New York.
So, yes, that is all exciting news. However, what it means for the near future isn’t entirely clear. As of right now, there is limited availability of the vaccines, and they are being rolled out in phases based on priority and need. If you’re not an essential worker or over the age of 65, you may need to wait a while to get vaccinated.
“It is difficult to predict when most Americans will have the opportunity to receive the COVID-19 vaccine, but late spring or early summer seems like a reasonable estimate,” says Richard Watkins, MD, an infectious disease physician and professor of medicine at the Northeast Ohio Medical University.
Adds Dr. Sellick, “Hopefully, a good chunk of the population will be immunized by the summer.”
Is the COVID-19 pandemic going to continue getting worse this winter before it gets better?
COVID-19 has shown that it can spread regardless of the weather. Summertime even brought surges in areas of the country that are especially hot, like Florida, Texas, and Southern California.
Changing seasons tend to have *less* of an impact on new viruses, says Sandra Kesh, MD, an infectious disease specialist and deputy medical director at Westmed Medical Group in Purchase, New York, so you can still get sick outside of the typical winter season. And, remember: This is global, so it’s always winter somewhere.
Unfortunately, things are expected to get worse this winter before it gets better, especially after people gathered together for the holidays. “It is likely we will hit a peak of cases in January because of the December holiday season,” Dr. Watkins says.
Dr. Sellick agrees. “We had a big bump in cases after Thanksgiving. If people gather the same way over the holidays and New Year’s, we’re going to see another jump,” he says.
So what might happen with the novel coronavirus in the next few months, then?
“Because this is a new virus, those who have not been infected (the vast majority of the world) have no immunity to it,” says Dr. Kesh. That’s why if enough people in a community get sick at the same time, it overwhelms our health care resources and disrupts the everyday processes in life we all rely on like going to school, work, shopping centers, and public gatherings, she explains.


Don’t be surprised if events continue to stay canceled or postponed until vaccine uptake is widespread—and expect to stay inside, save for essential outings and activities, and limit contact with others for the foreseeable future. The more people who stick to the rules in their area, the better off we’ll all be, experts agree.
Will people have to practice social distancing until the end of the pandemic?
Yup. The pandemic might not be formally declared over for a while. When social distancing isn’t possible, it’s crucial to wear a mask and avoid congregating in large groups—especially indoors, Dr. Yancy says. “These are simple things, and research has shown they work,” he adds.
Overall, Dr. Sellick says you should keep on practicing known ways to prevent the spread of COVID-19 until public health officials say otherwise.
Truth is, you’ll have to go with the flow as COVID-19 continues on, as the future remains unknown. But ultimately, the future of the coronavirus pandemic depends on how we respond to it together, and there’s plenty you can do to help, experts agree.
Follow the rules regarding social distancing, wear a mask when you’re around people who aren’t in your household, stay calm (as much as you can!), and stick to the basics, too. Wash your hands often, keep them away from your face, know what symptoms to look out for, do your best to be especially vigilant around at-risk populations (like the elderly and immune-compromised), and encourage your friends and family to follow suit.
Source: Read Full Article


