Magnetic Resonance Imaging (MRI) has been used to detect instances of neurological disorders in patients across hundreds of studies since the first images were produced by the method in the early 1970s.
Many patients and medical scientists have benefited from its use since these early days of MRI, with ever-more detailed images being produced as the method has been refined, leading to increased understanding of numerous conditions that affect the brain.
Individuals on the autism spectrum have particularly benefited from the early and detailed detection and analysis that MRI has provided since its invention, and the information gleaned by clinical studies. Medical use of the machinery and technique has provided invaluable insight into the processes that lead to these conditions.
Autism spectrum disorder
Autism spectrum disorder is a term for a family of neurological conditions, which can be hereditary. The term “spectrum” applies to the range of symptoms and severity across these disorders.
 Image Credits: PhotoUG / Shutterstock.com
Image Credits: PhotoUG / Shutterstock.com
Conditions now considered to be within the autism spectrum that were previously considered unrelated include Asperger’s syndrome and childhood degenerative disorder. Asperger’s syndrome is generally considered to be at the mild end of the spectrum.
Autism spectrum disorder impacts the individual in a number of ways. The disorder develops early in life and symptoms are apparent usually within the first year, but a child may develop normally for this period and then may seem to “regress” as symptoms develop between 18 and 24 months.
Early symptoms include reduced eye contact, indifference to those around them including caregivers, and a lack of response to their name. Children may become aggressive or withdrawn and lose language skills if the condition develops later in infancy.
Core symptoms include problems with social reciprocity, nonverbal communication, sensory abnormalities, and insistence on “sameness”.
Peripheral symptoms include behavioral comorbidities (hyperactivity/impulsivity, anxiety), cognitive comorbidities (language impairment, intellectual disability), and medical comorbidities (constipation, seizure disorders, hyper-serotonemia, developmental macrocephaly.) Genetic markers include fragile X disorders and rare variants include NRXN1 and NLGN4.
Each autistic person has unique patterns of behavior. Additionally, social stigmas exist for autistic people, and these can have profound effects on them that come from a lack of understanding of their needs and wants and the conditions that fall within the autism spectrum. There continues to be conflicting and unhelpful information from various institutions, which only serves to further push social stigmas upon the autistic person.
The use of MRI for the detection of autism: new frontiers in diagnosis
Being a condition that has a neurological basis, it follows that using techniques that can image affected parts of the brain are advantageous in studies upon, and diagnosis of, autism spectrum disorders. Early detection of the neurological markers can lead to more accurate diagnosis, and hence more appropriate care and treatment. Recent research has been carried out into the use of MRI for this purpose.
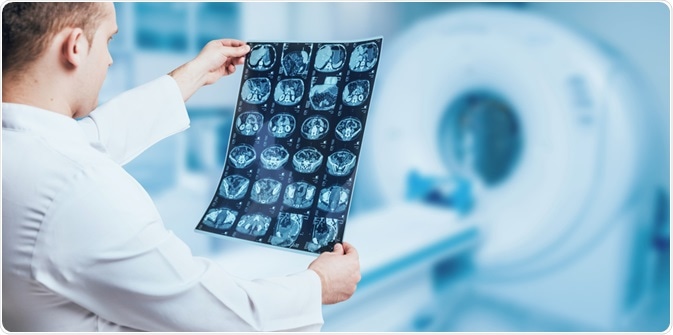 Image Credits: Roman Zaiets / Shutterstock.com
Image Credits: Roman Zaiets / Shutterstock.com
In a 2017 proof of concept study published in Nature and widely reported in various media outlets, a team led by Heather Cody Hazlett with researchers from the Universities of North Carolina, Minnesota, and New York University used data from the Infant Brain Imaging Study (IBIS), which included MRI scans.
The study aimed to investigate whether ASD could be detected around six months in high-risk children with a family history before symptoms developed. The team also wanted to see if these brain changes could be detected in children at low risk of developing ASD.
The team analyzed data for 106 high-risk and 42 low-risk children to look for any link between the diagnosis of ASD at 24 months and the appearance of clinical symptoms in early infancy. The team found that in 15 infants who later went on to be diagnosed with ASD there were noticeable brain changes.
These included cortical surface area expansion at around 6-12 months of age and brain overgrowth between 12 and 24 months. However, there was no difference in total brain volume growth at the 6-12 month stage of development between high and low-risk children.
The team concluded that early brain changes occurred during the period where autistic behaviors and symptoms first emerge in infants and that early postnatal hyper expansion of cortical surface areas seems to be one of the key indicators of brain development in autistic children.
Summary
In conclusion, the study carried out in 2017 provides positive proof of concept that MRI scans can potentially aid earlier diagnosis of infants with ASD.
However, studies including more data would be needed to see if these physiological changes are present in all children with autistic spectrum disorder. Also, a high degree of accuracy in tests is necessary to prevent under- or over-diagnosis of ASD in children.
More studies in this area are ongoing currently and the use of MRI scans to provide a diagnostic tool for early detection of ASD before the onset of symptoms could prove invaluable for clinical science and the proper care and treatment of autistic people throughout their lives.
References
Hewiston, Laura (2013) Scientific challenges in developing biological markers for autism Researchgate.net. Available from: https://www.researchgate.net/publication/269626244_Scientific_challenges_in_developing_biological_markers_for_autism
Hazlett, H.C. et al. (2017) Early brain development in infants at high risk of autism spectrum disorder Nature Vol. 542. Available from: https://www.nature.com/articles/nature21369.epdf
Autism Spectrum Disorder – Mayo Clinic. Available from: https://www.mayoclinic.org/diseases-conditions/autism-spectrum-disorder/symptoms-causes/syc-20352928
Further Reading
- All Clinical Imaging Content
- Single Photon Emission Computed Tomography (SPECT)
- Positron Emission Tomography
- Whole-Body Low-Dose Computed Tomography (WBLDCT)
Last Updated: Apr 7, 2020

Written by
Reginald Davey
Reg Davey is a freelance copywriter and editor based in Nottingham in the United Kingdom. Writing for News Medical represents the coming together of various interests and fields he has been interested and involved in over the years, including Microbiology, Biomedical Sciences, and Environmental Science.
Source: Read Full Article
