- Currently approved COVID-19 vaccines provide protection against symptomatic Omicron infection but the protection wanes quickly, highlighting the need for novel or updated COVID-19 vaccines.
- A recent animal study shows that using a skin patch to deliver a COVID-19 vaccine candidate effectively produced a robust neutralizing antibody response against both the original wild-type SARS-CoV-2 virus and all tested variants, including Omicron.
- Notably, the skin patch produced a larger neutralizing antibody response than an injection of the same vaccine under the skin using a needle and a syringe.
- The need for smaller amounts of vaccine, its stability at room temperature, and ease of use could make this skin patch-based vaccine an alternative in resource-limited nations.
A recent animal study shows that administering a genetically modified form of the SARS-CoV-2 spike protein using a skin patch produced a potent neutralizing antibody response against the Omicron and Delta variants.
Furthermore, when compared to it being injected intradermally (under the outermost skin layer, using a needle), it produced a higher immune response, suggesting that a skin patch vaccine may be more effective for delivery.
The study’s co-author Dr. David Muller, a virologist at the University of Queensland in Australia, says, “The patch technology has the potential to offer a new—and more effective—weapon in our arsenal, at a time where new variants are mutating at a rapid rate. The patches are not only more effective against emerging variants but are also far easier to administer than needle-based vaccines.”
The study appears in the journalVaccine.
Need for more COVID-19 vaccines
Currently approved COVID-19 vaccines train the body to elicit an immune response against the wild-type SARS-CoV-2 spike protein. The accumulation of mutations, including in the spike protein, has resulted in the emergence of new SARS-CoV-2 variants that can evade the immune response in vaccinated individuals.
For instance, fully vaccinated individuals tend to show a decline in neutralizing antibody levels against the Omicron variant. Neutralizing antibodies can bind to the spike protein and other SARS-CoV-2 proteins and prevent the coronavirus from infecting human cells.
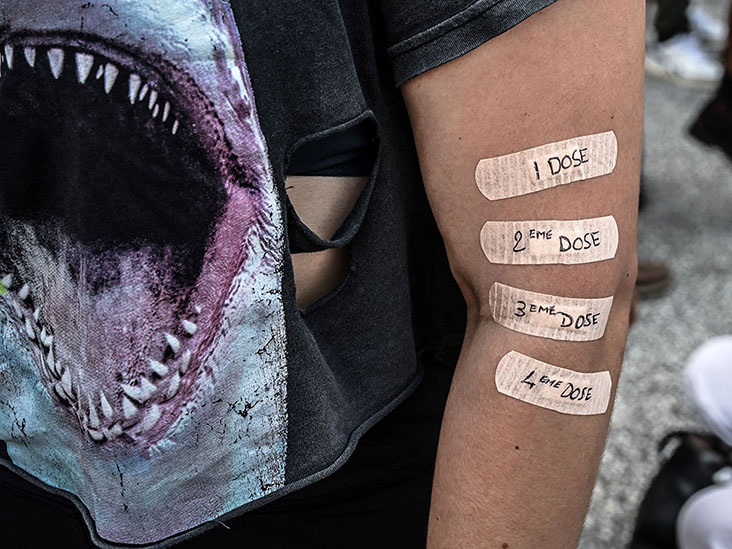
Notably, neutralizing antibody levels are associated with the extent of protection against a SARS-CoV-2 infection. Although booster shots are effective in eliciting a robust neutralizing antibody response against the Omicron variant, this response starts to wane after a few months.
This underscores the need for new vaccines that can confer broad protection against SARS-CoV-2 variants.
Moreover, currently approved vaccines need to be stored at low or ultra-low temperatures, posing challenges for the transportation and distribution of these vaccines to resource-limited countries.
How do intradermal vaccines work?
HexaPro, a vaccine with a genetically modified version of the SARS-CoV-2 spike protein, is one such vaccine candidate that could potentially address these issues. Unlike the wild-type spike protein, HexaPro is stable across a wide range of temperatures and can be stored at room temperature. The substitutions present in HexaPro also facilitate high-yield production of this protein at a low cost, making it a suitable vaccine candidate.
Researchers at the University of Queensland in Australia worked in collaboration with the Vaxxas biotechnology company to develop a needle-free COVID-19 vaccine in the form of a skin patch—coated with the HexaPro subunit vaccine candidate.
The skin patch, referred to as a high-density microarray patch (HD-MAP)— a small patch with microprojections —delivers HexaPro to the layers of the skin that contain high levels of antigen-presenting cells. These antigen-presenting cells process or break down foreign molecules, such as the spike protein, and display them to the immune cells to produce an immune response.
Due to the abundance of antigen-presenting cells in the skin, intradermal vaccination can elicit a more potent immune response with smaller quantities of vaccine than an intramuscular injection used for currently approved vaccines.
Are skin patch vaccines a new thing?
Intradermal vaccination has been used for a long time, but the methods used for intradermal delivery have shown certain shortcomings. For instance, intradermal vaccination using a conventional hypodermic needle requires high levels of skills and training, whereas newer methods have shown inconsistent results.
Microneedle skin patches involving tiny needles have also been used to deliver the vaccine intradermally, but the results have been similar to conventional intradermal injection. These studies have generally used microneedle patches consisting of a relatively low number of needles to administer the vaccine.
More recently, this approach has been modified to incorporate a larger number of densely-packed projections that are smaller in diameter than conventional microneedles. These projections are less likely to cause the death of immune cells while more precisely targeting the antigen-presenting cells.
For instance, the HexaPro vaccine patch consists of 5,000 solid microscopic projections arranged on a 1 square centimeter patch. The researchers had previously shown that mice who received the HexaPro protein subunit vaccine candidate via this skin patch had protection against COVID-19.
Moreover, the mice vaccinated via the skin patch also showed a robust neutralizing antibody response against the Alpha and Beta variants that were in circulation during that study.
In the present study, the researchers assessed whether the HexaPro skin patch could produce robust neutralizing antibodies against newer variants, including Omicron and Delta, in mice.
For that, the researchers compared neutralizing antibody levels against several SARS-CoV-2 variants after the delivery of HexaPro via the skin patch and with that after a conventional intradermal injection.
Skin patches vs. intradermal vaccines
The researchers administered two doses of HexaPro to adult mice at an interval of 3 weeks using either the skin patch or a needle and syringe. The researchers then collected serum from the mice three weeks after the last vaccine dose to evaluate the neutralizing antibody response.
The mice who received HexaPro through the skin patch elicited a robust neutralizing antibody response against all tested variants of SARS-CoV-2 — ancestral, Gamma, Delta, Kappa, Lambda and Omicron. In contrast, those who received the intradermal injection of HexaPro produced very low or negligible levels of neutralizing antibodies against these variants.
Using an adjuvant, or helper ingredient, with HexaPro also resulted in a larger neutralizing antibody response than HexaPro alone, regardless of whether the vaccine was administered with a needle or via a skin patch.
However, delivering Hexapro and the adjuvant via the skin patch still resulted in higher neutralizing antibody levels than conventional intradermal injection.
These results are consistent with previous studies involving other types of vaccines administered using the skin patch. The study’s co-author, Dr. Christopher McMillan, a researcher at the University of Queensland, says:
“So far, every vaccine type we have tested through the patch, including subunit, DNA, inactivated virus, and conjugate produces superior immune responses compared to traditional needle vaccination methods.”
The researchers are now planning to conduct clinical trials to assess the effectiveness of the Hexapro skin patch in humans.
Skepticism about its utility
Despite these results, there are some doubts about the utility of this approach.
Dr. Martin Bachmann, an immunologist at the University of Bern, Switzerland, said:
“This is a potentially interesting paper but may not be that relevant for real-life applications because using patches for immunization has been notoriously difficult in humans and pretty much failed as a platform so far. Avoiding needles also seems to me less of an issue for SARS-CoV-2.”
He said research on needle-free solutions for COVID-19 had already produced better alternatives, such as intranasal vaccines.
“We and others published recently that intranasal needle for application was potentially attractive, but mostly not for ease of use but rather because you additionally induce mucosal immune responses, mostly IgA,” he pointed out.
Source: Read Full Article