Research conducted at the Sharon Eccles Steele Center for Translational Medicine (SCTM) at the University of Utah’s John A. Moran Eye Center explains why people carrying a block of genetic variants strongly associated with the development of age-related macular degeneration (AMD) may develop the disease and identifies a potential therapeutic pathway for slowing or even reversing disease progression.
AMD is a major cause of irreversible blindness worldwide and the leading cause of blindness for Americans aged 55 and over. Following more than 15 years of research that has employed an extensive repository of donated human ocular tissues, scientists found that HtrA1 protein normally increases with age in the eye at the retinal pigmented epithelium (RPE)-Bruch’s membrane interface, helping to maintain the normal function of this region. The RPE is a cell layer that delivers nutrients to and removes waste from the retina’s light-sensitive photoreceptor cells.
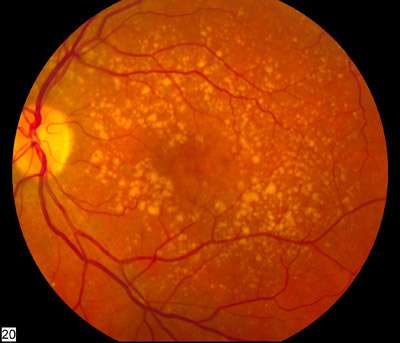
These new data show this is not the case in individuals with AMD-associated risk variants located on chromosome 10. These variants were found to impair expression of the HTRA1 gene by the RPE, resulting in an approximately 50 percent reduction of HtrA1 protein levels at the RPE-Bruch’s membrane interface during aging. The failure to produce adequate levels of HtrA1 protein disrupts this key region of the eye and is associated with AMD-associated pathologies, including the deposition of abnormal deposits and the development of abnormal blood vessels.
These findings, coming from the laboratory of SCTM Executive Director Gregory S. Hageman, Ph.D., represent the first explanation of the essential role of HtrA1 in maintaining ocular health and contradict literature previously published by others. They are anticipated to inform the development of novel therapies for chromosome 10-directed AMD.
These research data will appear the week of July 19, 2021, in the Proceedings of the National Academy of Sciences of the United States of America (PNAS): “Chromosome 10q26-Driven Age-related Macular Degeneration is Associated with Reduced Levels of HTRA1 in Human Retinal Pigment Epithelium.”
Lead author Brandi L. Williams, Ph.D., said her team found significantly reduced levels of HTRA1 messenger ribonucleic acid (mRNA) in the RPE and secreted HtrA1 protein at the RPE-Bruch’s membrane interface. Reduced HTRA1 expression was found to be risk allele-specific, but only in the RPE and not in the neural retina or choroid. Notably, the team also narrowed a large genetic region of AMD-associated chromosome 10 to a much smaller causal region, which likely directs the reduced expression of HTRA1.
“Our findings are significant because they suggest that HtrA1 normally maintains the integrity of the RPE-Bruch’s membrane interface during the aging process by, in essence, turning over extracellular material and preventing abnormal deposits—including basal laminar deposits—from accumulating between the RPE and Bruch’s membrane,” said Williams. “Earlier unpublished SCTM studies documented a significant association between chromosome 10 and the formation of basal laminar deposits. Viewing HtrA1 as protective runs contrary to what one might expect because elevation of HtrA1 protein is thought to be a contributing factor in some diseases such as osteoarthritis.”
Access to a unique repository of more than 8,000 pairs of donated human eyes was essential to this study since there are no animal models that accurately mimic the biology of chromosome 10-directed AMD. This critical resource allowed the SCTM team to compare HTRA1 expression in eyes derived from donors with and without chromosome 10-associated risk genotypes.
“We were able to generate these exciting results thanks to our eye donors and their families,” said Hageman. “We are so extremely grateful for their precious gifts.”
The SCTM team conducted a number of difficult and time-consuming experiments to reach their groundbreaking conclusions, which contradict previously published literature reporting either no difference or elevated levels of HtrA1 in human ocular tissues or blood. Hageman pointed out that “those particular studies employed too few samples and the analyses were performed using neural retina and white blood cells, rather than RPE-Bruch’s membrane, which is the primary site of AMD pathogenesis.”
“Unfortunately, data generated by prior studies have led to the development and testing of therapies—some of which are currently in human clinical trials—designed to reduce overall levels of HtrA1, an approach that may exacerbate AMD progression,” said Hageman. “Our team has been tireless in its pursuit of accuracy, conducting many extremely difficult experiments to generate these data. They persevered year after year, and I couldn’t be more excited about the data and the scientific acumen of this talented team.”
Williams said the research will have a broad impact.
“These data should be important to the entire field and to patients with this devastating disease,” she said, “especially in light of developing therapeutic technologies to correct genes by excising the defected region and repairing it.”
SCTM scientists and clinicians are now focused on the development of a therapy for chromosome 10-directed AMD. They have also developed a potential therapy for individuals at risk for AMD due to abnormal genes lying on chromosome 1. Together, chromosomes 1 and 10 account for more than 50 percent of genetic risk for developing AMD.
This is Hageman’s second publication in PNAS related to the major genetic underpinnings of AMD. In 2005, a landmark paper revealed that genetic variants and haplotypes in the Complement Factor H and related genes on chromosome 1 predispose individuals to AMD.
“When Dr. Hageman started his AMD-related research nearly 30 years ago, he was a marine biologist who decided to shift gears and investigate AMD at a time when this horrible, blinding disease was simply accepted as something no one could do anything about,” said Randall J Olson, MD, Moran Eye Center CEO and Distinguished Professor of Ophthalmology and Visual Sciences. “He didn’t accept that. I didn’t accept that. Thus, we created the SCTM as a unique academic model designed to quickly turn discoveries into therapies through partnerships with philanthropists and industry as well as national and international scientific collaborators.”
A major gene expression study conducted as part of a research and development collaboration with Allergan in 2014 employed various ocular tissues and blood cells from over 700 donors and patients, generated about 9.2 billion data points, and revealed new insights relating to the biology of gene-directed AMD.
Source: Read Full Article
