Cuomo, de Blasio leadership styles are conflicting: Don Peebles
National Real Estate developer Don Peebles discusses how New York Gov. Andrew Cuomo and New York City Mayor Bill de Blasio are in conflict, causing a sense of
New York leaders faced an unanticipated crisis as the new coronavirus overwhelmed the nation's largest city. Their response was marred by missed warning signs and policies that many health-care workers say put residents at greater risk and led to unnecessary deaths.
Continue Reading Below
In the first few days of March, Gov. Andrew Cuomo and Mayor Bill de Blasio assured New Yorkers things were under control. On March 2, Mr. de Blasio tweeted that people should go see a movie.
Only after the disease had gripped the city's low-income neighborhoods in early March did Gov. Cuomo and Mayor de Blasio mobilize public and private hospitals to create more beds and intensive-care units. The hasty expansion that ensued, led by New York government leaders and hospital administrators, produced mistakes that helped worsen the crisis, health-care workers say.
New York Gov. Andrew Cuomo speaks during a news conference against a backdrop of medical supplies at the Jacob Javits Center that will house a temporary hospital in response to the COVID-19 outbreak, Tuesday, March 24, 2020, in New York. Cuomo sounde The virus has hit New York harder than any other state, cutting through its densely populated urban neighborhoods and devastating the economy. New York state's death toll of 30,575 accounted for 7% of the world's deaths and 27% of American deaths as of June 11, according to Johns Hopkins University data. VARNEY RIPS CUOMO OVER CORONAVIRUS RESPONSE: 'NEW YORK CITY IS A MESS' The Wall Street Journal talked to nearly 90 front-line doctors, nurses, health-care workers, hospital administrators and government officials, and reviewed emails, legal documents and memos, to analyze what went wrong. Among the missteps they identify: — Improper patient transfers. Some patients were too sick to have been transferred between hospitals. Squabbling between the Cuomo and de Blasio administrations contributed to an uncoordinated effort. — Insufficient isolation protocols. Hospitals often mixed infected patients with the uninfected early on, and the virus spread to non-Covid-19 units. — Inadequate staff planning. Hospitals added hundreds of intensive-care beds but not always enough trained staff, leading to improper treatments and overlooked patients dying alone. — Mixed messages. State, city government and hospital officials kept shifting guidelines about when exposed and ill front-line workers should return to work. — Overreliance on government sources for key equipment. Hospitals turned to the state and federal government for hundreds of ventilators, but many were faulty or inadequate. — Procurement-planning gaps. While leaders focused attention on procuring ventilators, hospitals didn't always provide for adequate supplies of critical resources including oxygen, vital-signs monitors and dialysis machines. — Incomplete staff-protection policies. Many hospitals provided staff with insufficient protective equipment and testing. A patient is transferred from Elmhurst Hospital Center to a waiting ambulance during the current coronavirus outbreak, Tuesday, April 7, 2020, in New York. New York Gov. Andrew Cuomo said last week that the city’s overtaxed hospitals could move patie A spokeswoman for Mr. de Blasio, Freddi Goldstein, and a member of Mr. Cuomo's virus task force, Gareth Rhodes, said the city and state did everything they could to increase hospital capacity and enhance social distancing once the risk became clear. "Ultimately our hospitals withstood the pressure and our doctors and nurses delivered heroically," Ms. Goldstein said. Kenneth Raske, president of the Greater New York Hospital Association, defended the state and hospitals' response as remarkable considering the "wartime conditions," adding: "We have a large, very sophisticated hospital system. It took us to the breaking point." CUOMO'S OFFICE ABUSING POWER THROUGH CORONAVIRUS CLOSURES: LAWSUIT Under normal protocol, only stable patients typically would be transferred, but these people came in with "one foot in the grave," said Dr. David Buziashvili, who worked many shifts at Bellevue hospital, part of the city's public system, NYC Health + Hospitals. On one shift there, he was alarmed to see 10 new transfers in beds with little medical information, he said. "That is not how it should be done, and it is not safe for the patient at all." TRUMP, CUOMO WAR ERUPTS OVER CORONAVIRUS RESPONSE Avery Cohen, a City Hall spokeswoman, blamed the state for denying a request from the city to establish a centralized hub, called a Healthcare Evacuation Call Center, that would have helped better coordinate transfers between hospitals, whether they were private or public. "We were grasping for every tool at our disposal to save as many lives as possible." Ms. Cohen said. "The state was not interested." Dani Lever, a spokeswoman for the governor, said that system wasn't designed for individual patient transfers. She said a state transfer system was created in late March after hundreds of open beds near harder-hit New York City hospitals had gone unnoticed. Extraordinary outbreak The New York state outbreak was extraordinary, and much of the disarray in its hospitals from mid-March on traced to impacts few had anticipated, including the federal government. The impact was made worse because the city went into the pandemic less prepared than it could have been. The city hospital system has long been considered underfunded. Private hospitals in the outer boroughs, particularly Queens, had closed over the years. New York hospitals had long ignored alarms raised by the nurses' union and respiratory therapists about insufficient staffing levels, according to nurses and respiratory therapists at several city hospitals. A contributing factor was New York leaders' delayed reaction. Early signs of the virus's arrival — including a rise in patients with flulike symptoms visiting hospitals — went largely uninvestigated by hospital, state and city officials. The city health department was limiting testing primarily to travelers from China, following the federal government's lead. Throughout February in calls with hospitals, the city health department played down the possibility that the virus could spread through the air or by asymptomatic people. In early March at Health + Hospitals' Elmhurst, Dr. Chad Meyers and his colleagues in the emergency room worried they were missing community spread of Covid-19. But when they called the city's health department to get patients tested, it rejected for testing even many patients who satisfied the criteria, Dr. Meyers said, leading to "often protracted and unproductive calls" with the department. Hospital, city and state officials said they were relying on the federal government for testing capability and were limited by criteria set by the Centers for Disease Control and Prevention on whom they could test. Jason McDonald, a CDC spokesman, said: "CDC testing guidance has always allowed for clinical discretion. So, while we set guidelines, states and health-care providers have had the flexibility to determine who to test." In an April interview, Health + Hospitals Chief Executive Mitchell Katz said the system prepared as best it could, given the difficulties of building additional space in already-full hospitals. In a May 15 city-council meeting, he said he should have acted quicker. While leaders in states like California and Ohio acted quickly to contain the spread, Messrs. Cuomo and de Blasio delayed taking measures to close the state and city even as the number of cases swelled, despite warnings from doctors, nurses and schoolteachers. California issued a statewide lockdown with 1,005 cases as of March 19, while New York remained open with 5,704 cases, according to updated Johns Hopkins data. Even after New York announced its first coronavirus case on March 1, the city health department was advising New Yorkers they were more likely to get the flu. "I speak for the mayor also on this one — we think we have the best health-care system on the planet," Mr. Cuomo said at a March 2 news conference. Five days later, Mr. Cuomo declared a state of emergency, but medical and emergency-response experts worried the city and state administrations still weren't taking matters seriously enough. Richard Serino, an adviser to the city and a former deputy administrator at the Federal Emergency Management Agency, told a senior aide to Mr. de Blasio early on March 13 that he was "concerned about the cavalier attitude of the hospital community" in the city, especially compared with other cities like Boston, according to an email. Officials with the city's emergency-management agency agreed, according to people familiar with the matter. Mr. Serino in April said he didn't recall the email and praised the city's response. March 13 became a turning point after it became clear there was community spread from one man in a New York City suburb. The city went from planning for a future crisis to responding to one already there. Two days later, when Mr. de Blasio said known New York City cases had already ballooned past 300, he reluctantly closed schools. Los Angeles closed schools around the same time with about 50 cases, according to Johns Hopkins data. By March 20, the ICU of the Northwell Health system's Long Island Jewish Medical Center in Queens was overflowing, and Health + Hospitals' Elmhurst had to borrow ventilators from a sister hospital to keep up, the Journal reported that month. The governor ordered most of New York be put under quarantine two days later. On March 23, Mr. Cuomo ordered hospitals to increase capacity to treat Covid-19 by 50%, anticipating the need for 140,000 new beds. When hospital executives asked where they would get staffing, beds and protective gear, state officials told them to "do your best," said a hospital executive familiar with the conversation. Ms. Lever, the governor's spokeswoman, said the state offered every hospital access to 90,000 volunteer health-care workers and to a central inventory system for the resources and equipment they needed to fight the virus. Once they realized how widespread the virus had become, Messrs. Cuomo and de Blasio sparred with President Trump to procure more equipment and sought out creative ways to jump-start ventilator production. Both were frank about the gravity of the illness in daily public briefings, and Mr. Cuomo's job-performance rating soared. Mr. de Blasio focused on inequities within the city, establishing a food program, providing meals at city schools and using out-of-work taxi and for-hire vehicle drivers to make deliveries to homebound residents. 'Absolute crisis' Among the missteps that would make matters worse after mid-March, health-care workers said, was that government officials and hospital administrators failed to create adequate plans to provide the needed staff as they expanded beds into operating theaters, old auditoriums and lobbies. "Creating beds isn't the most difficult thing," said Northwell CEO Michael Dowling. "The issues that get complicated with the creation of beds is the staffing. This isn't like you can put any staff on any bed at any place." The crisis would eventually peak at nearly 19,000 hospitalizations, but even that number overloaded the system. As Covid-19 patients flooded into NewYork-Presbyterian/Columbia, the private hospital created new pop-up ICUs. The inadequacy of staffing levels quickly became clear in one operating-room-turned-ICU, according to medical staff there and emails residents sent attending physicians. Garbage in the makeshift 80-bed unit overflowed with contaminated needles, masks and gowns. Urine and blood stains were at times found on the ground and equipment, according to the workers and emails. "The scope of patient needs compared with the training and resources available presented an absolute crisis," said Julia Symborski, a nurse who worked in the new ICU. "You can magically make an ICU appear, but you can't make staff appear immediately." A NewYork-Presbyterian spokeswoman, Kate Spaziani, defended the hospital system's response to the "unprecedented challenges, many anticipated, others unexpected." Across New York, hospitals sometimes mismanaged the staff they did have and were slow to staff up with additional critical-care nurses and key respiratory therapists to manage the growing number of patients on ventilators, dozens of front-line workers said. It isn't that there weren't staff available nationwide: Brian Cleary, CEO of Krucial Staffing, an agency Health + Hospitals tapped to send 4,000 medical staff during the crisis, said it could have sent in 6,000 more "without blinking." A Health + Hospitals spokeswoman said the hospital began securing additional staffing in early January and Krucial "does not encompass the full scope of the assistance we sought from outside groups." In some cases, available doctors and trained critical-care nurses said hospitals failed to reduce the bureaucracy to get them in quickly. Chelsea Walsh, a traveling nurse from Hawaii, said red tape from NewYork-Presbyterian — including a request for her to take a drug test — discouraged her from working there, so she took shifts elsewhere in the city. "I couldn't work for a hospital in the middle of a crisis that wanted me to do paperwork before I help save someone's life. The paperwork and the administration's rules delayed a lot of care." While travel nurses arrived at Bellevue and other locations, "a lot of them had no experience whatsoever," said Laura Jaramillo, a Bellevue ER nurse. She had to spend time training some of them while also juggling patient care. The Health + Hospitals spokeswoman said new staffers were "formally trained to cover the areas they were posted in." In the new operating-room ICU at NewYork-Presbyterian/Columbia, one respiratory therapist at times cared for over 80 patients a shift, according to workers and emails; seeing about 10 a shift is typical in normal times, respiratory therapists said. Overworked staffers there weren't able to suction mucus out of patients' lungs often enough, resulting in patient complications, according to the workers and emails. Intubated patients' lips were bleeding and many developed sores on their backs, called pressure ulcers, from not being turned enough. "We are not running these ICUs safely or appropriately," a Columbia resident wrote in an email to the attending physicians. "The emotional burden of working in these sci-fi-movie-gone-wrong ICUs is through the roof." NewYork-Presbyterian's Ms. Spaziani said the hospital system began recruiting additional staff in February and ended up with more than 2,850 volunteers and temporary front-line staff, including 150 additional respiratory therapists. Joji Thadathil, a Health + Hospitals Elmhurst respiratory therapist, estimated that more staffing and better equipment could have saved 30% to 40% of Covid-19 patients who died there. Rio Flores, a respiratory therapist, said he documented 50 patients who died in part due to improper ventilator settings by untrained staff and state-provided ventilators with limited functionality at the NewYork-Presbyterian system's Lower Manhattan hospital. Respiratory therapy is a specialized job that requires a license and at least two years of training. The Health + Hospitals spokeswoman said the system "mobilized quickly to shift staff…and equipment to the hardest hit hospitals." NewYork-Presbyterian's Ms. Spaziani said the hospital received no such reports about ventilator malfunctions. The staffing shortages led to hospitals losing track at times of admitted patients. At Brookdale University Hospital Medical Center in Brooklyn, a family member called the ER to inquire about their mother in her 80s. An ER doctor said that when he looked the patient up, he realized she had died two days prior. "This is happening daily," the doctor said during the peak. Brookdale spokesman Khari Edwards said the hospital's staff "did their absolute best to provide care to those in need during this pandemic." Air supply During the surge's early days, Mr. Cuomo, Mr. de Blasio and hospital officials often talked publicly about the urgent need for ventilators. That procurement emphasis, some medical workers said, overshadowed staffing and other vital needs like oxygen and oxygen monitors. Supplemental oxygen became especially important to keep Covid-19 patients breathing and off the dwindling supply of ventilators, especially once it became clear most patients on ventilators were dying. At least eight New York City hospitals experienced problems with their oxygen supplies, said some health-care workers and state officials. It wasn't that oxygen wasn't available on the market, said some gas experts. Kimberly Menard, a spokeswoman for Pennsylvania-based Airgas, a unit of France's Air Liquide SA, said that while the company saw increased demand from hospitals, it "has not experienced an inability to supply requested medical oxygen anywhere in the U.S." The problem was that the state, city and hospitals' action plans didn't quickly step up their ability to procure and dole out enough oxygen and related supplies, including vital-signs monitors to keep track of patients. At Health + Hospitals' Lincoln in the Bronx, a severe oxygen shortage hit mid-surge, said doctors there including Dr. Dasol Kang. He said some Covid-19 patients, including a woman in her 50s and a man in his late 40s, languished without portable oxygen tanks, worsening so much they needed intubation and later died. The Health + Hospitals spokeswoman said the hospital didn't experience a shortage and never rationed oxygen. The facility nearly doubled its daily oxygen supply in response to the surge, she said. Mr. Dowling, Northwell's CEO, said the hospital system was using some 50 times more oxygen than ever before and ran into pressure points. "Did we at a few locations have to address an oxygen issue? Yes. Did we run out of oxygen? No." With scores of patients needing ICU-level care, hospitals ran short of the vital-signs machines needed to effectively monitor such patients and of the staff needed to keep track of them. Covid-19 patients gasping for breath sometimes weren't being properly monitored as they lay hooked up to oxygen, and sometimes died without anyone's knowing, said doctors and nurses from at least eight New York City hospitals. Often this happened when patients, feeling suffocated, pulled off their oxygen masks. Jenna Smarrella, a traveling nurse from Ohio, said she had a patient in his 80s who seemed stable at Health + Hospitals' Harlem. When she came back, he had removed his mask and was dead. "If he was on a monitor," she said, "I would have known." The Health + Hospitals spokeswoman said it had an ample supply of monitors to track patients continuously. Medtronic PLC, a medical-equipment company that creates respiratory-monitoring systems for hospitals, said there was no shortage of such equipment and it was able to meet increased demand from New York during that time frame. Dräger Inc., another such company, said it was "able to meet patient monitoring demand and did not encounter monitoring shortages in 2020." Despite emphasizing ventilators, the Cuomo and de Blasio administrations and hospital leaders didn't ensure a supply of quality equipment, health-care workers said. A big surprise to doctors and nurses was the number of shoddy ventilators, called LTVs, distributed by the state from its own stockpile and by both the state and city from the federal government's reserve. Several health-care workers, including Mr. Thadathil, the Elmhurst respiratory therapist, and Dr. Meyers, the ER physician, said the government ventilators were old and many patients worsened on them, leading to collapsed lungs and other complications. Because LTV alarms often rang, "it's impossible to know if one of those vents actually is trying to indicate something dangerous is happening," Dr. Meyers said. The Health + Hospitals spokeswoman said many state ventilators "were not 'ready to go' when they came." She said the system did additional maintenance before they could be used on patients. Ms. Lever, the governor's spokeswoman, said the state tested every ventilator before sending them to hospitals and received no complaints about faulty ventilators. The government and hospital action plans also failed to procure enough equipment including IV pumps that control medicine flow, and dialysis machines — even though, by early March, it was evident from Chinese data that kidney failure was a main issue Covid-19 patients face. At Health + Hospitals Lincoln's ICU during the first two weeks of April, Dr. Donya Bani Hani said she saw a Covid-19 patient die every day or two because of complications dialysis might have prevented though some were worsening and might have died anyway. At Bellevue's ICUs, at least 10 patients died because they couldn't get dialysis in time, a doctor there said. Another physician there, Dr. Buziashvili, said he saw a patient aged in the 50s die waiting in line for a machine. Still, he said "Bellevue did well to adapt and restructure appropriately as we gained more knowledge on the virus." The system's spokeswoman said no patient died due to lack of dialysis treatment. Transfer squabble The discord between the Cuomo and de Blasio administrations, which have a long history of conflict, complicated patient transfers. When New York City's Office of Emergency Management realized massive mobilization would be needed to coordinate transferring hundreds of Covid-19 patients from overwhelmed hospitals, the mayor's administration sought the state's help to activate a centralized evacuation hub previously used for emergencies like superstorm Sandy, according to city officials. Twice, the state's department of health denied the request, the officials said. When the state gave the green light on March 26, the hub was used to transport patients only to Javits Center and the USNS Comfort Navy ship, the officials said — facilities set up with the federal government that ended up disappointing hospital executives because they weren't initially built for critical care or to take Covid-19 patients and eventually took only mild to moderately ill Covid patients. Ms. Lever, the spokeswoman for the governor, said that throughout March, the city publicly made clear its preference was to handle patient transfers on its own or not move patients at all. After state officials found hundreds of open hospital beds were going unnoticed while other hospitals were overrun, Mr. Cuomo announced a state-run program on March 30 to coordinate beds, equipment and staff. An ad hoc team of agency officials and top aides to Mr. Cuomo put together a mapping tool and began calling facilities that were close to capacity and helping coordinate transfers, said Jim Malatras, the president of SUNY Empire State College who has been advising Mr. Cuomo's pandemic response. But the system didn't supervise the transfer of medical records about patients or follow up on their conditions once they were moved, he said. "You were trying to manage volume," Mr. Malatras said, "not necessarily the individual patient need." State officials said the transfer system ultimately helped save lives, such as when oxygen-tank lines began to freeze because they were overloaded with ventilators at Flushing Hospital Medical Center and Jamaica Hospital Medical Center. The state was able to coordinate 26 transfers within an hour to hospitals in the city and upstate. A spokesman for the hospitals confirmed the episode but declined to comment further. The state didn't coordinate transfers inside hospital systems, where inadequate coordination made matters worse for some Covid-19 patients. In Health + Hospitals Bellevue's emergency room, ambulances hauled in about 30 transfers nearly every day for a few weeks during the surge from hospitals like the system's Elmhurst, Lincoln and Woodhull. Often, the patients arrived in critical condition — something unusual in normal times — several nurses and doctors at Bellevue said. Some of those died soon after arriving. One April evening, ER nurse George Good had just toe-tagged a corpse when he saw a newly transferred man in his mid-60s roll in with a breathing tube. He was "hanging onto life by a thread," Mr. Good said, then his heart rate started to plummet: 63, 43, 32, nothing. Mr. Good said he saw some other transfers die soon after arriving in the ER. "It was just something we kind of had to deal with." Three transfers from Health + Hospitals' Woodhull in Brooklyn came in one night "coding" and in need of resuscitation within 30 minutes of getting there, another Bellevue doctor said. All three died. Under normal protocol, patients on the verge of death are rarely transferred. Dr. Buziashvili at Bellevue was disturbed that at times the transfers lacked records of prior treatment — records that normally are a standard part of patient transfer. He had three or four "patient unknowns," arriving with no name. In one case, a family member came in to identify the patient. Health + Hospitals said it transferred about 850 patients during the crisis but declined to disclose how many transfers survived. "Covid patients were generally unstable, and their conditions changed rapidly regardless of area of care or transport," the system's spokeswoman said. Cross-infections As New York lurched into action in mid-March, shifting state, city and hospital policies sometimes put patients and medical staff at risk. Early on, most hospitals told staff to isolate suspected Covid-19 patients in rooms with negative air pressure to limit spread. But as patients flooded in, hospitals including Maimonides Medical Center, Health + Hospitals' Bellevue and Harlem, and Northwell's Staten Island University Hospital housed suspected Covid-19 patients together, sometimes side-by-side or in the same vicinity as confirmed Covid-19 patients, health-care workers there said. Sick patients likely infected some neighbors in the days it sometimes took to get test results, they said. Hospital administrators in February had said they had enough isolation rooms to deal with the crisis. When the scope became clearer in mid-March, health-care workers said, government and hospital leaders could have set up more negative-pressure areas with proper ventilation or field hospitals to take in and quickly isolate patients suspected of having Covid-19. The Health + Hospitals, Northwell and Maimonides spokespeople said they made every effort to isolate suspected Covid-19 patients based on symptoms but were thrown curveballs as patients presented with nontypical symptoms and space became constrained. Health + Hospitals' CEO, Dr. Katz, said he believed a crowded hospital was preferable to a field hospital: "I'd rather have patients in hallways in a hospital than have them be at an armory." It didn't help that New York City, state government and hospital officials, often relying on CDC guidance, kept shifting guidelines about when sick and exposed front-line workers should return to work — and didn't plan for thorough staff testing. Initially, the government and hospital officials recommended health-care workers with high-risk exposures quarantine for 14 days. Then the city on March 17 changed its guidance, recommending hospitals tell such workers they could keep working so long as they didn't show symptoms. Montefiore Medical Center passed that guidance along to workers in a March 18 memo. Some health-care workers there said they took that as an instruction to stay on the job. The city's guidance on testing further confused matters: "DO NOT TEST asymptomatic and/or exposed" workers, read a March 20 city memo to hospitals, citing supply shortages. The state on March 28 said workers who tested positive could return after seven days, so long as they were fever-free for 72 hours and their symptoms had improved. Hospitals didn't always follow the state's guideline, sometimes telling ill workers to return early, according to affidavits filed by nurses in a union lawsuit against the state health department. A New York County Supreme Court judge on May 28 dismissed the nurses' union's suit against the health department, saying it was beyond judicial review. Lincoln's Dr. Kang couldn't find a face shield before running in to help intubate a patient who was crashing. He soon tested positive and left work in late March. After two weeks, he said, hospital administrators told him to return if he didn't have severe symptoms. He was still coughing and couldn't smell anything but came back. Dr. Kang said he was shocked he wasn't retested although tests were available at the time. Spokespeople for hospitals including Health + Hospitals said they followed state, city and federal guidelines for their return-to-work policies. The CDC on March 17 was advising that confirmed Covid-positive health-care workers shouldn't return to work until they received a negative test and their symptoms had improved, according to a notice at the time from the Greater New York Hospital Association. On April 30, the CDC updated its guidance to say Covid-positive workers didn't necessarily need a negative test to return and could wait 10 days after symptoms first appeared and 72 hours after they abated. GET FOX BUSINESS ON THE GO BY CLICKING HERE PPE paucity Hospital officials said that, as early as January, they started to see signs there was a world-wide shortage of personal protective equipment, or PPE. But before the mid-March surge, many New York government and hospital leaders assured citizens there was enough PPE. Montefiore CEO Philip Ozuah said in a Feb. 7 memo to employees about coronavirus that "we are well prepared to meet this clinical challenge." A Montefiore spokeswoman, Elizabeth Kaledin, said: "At the time of this memo, Montefiore was making all efforts to acquire PPE." Many hospital administrators advised staffers in the first week of the mid-March surge that a thin surgical mask was enough to protect them from droplets produced by coughs. Later, they were told to wear the more robust N95 masks. Then the CDC said that, in a shortage, a covering like a bandanna could suffice. In televised conferences starting in late March, Mr. Cuomo repeatedly said New York had enough protective gear, based on assurances he was hearing from hospitals. But by then it was clear inside some hospital systems that efforts to procure PPE had fallen short, resulting in administrators scrambling mid-crisis. In mid-April, after hearing from distressed front-line workers, state officials realized some hospital supervisors and administrations were holding on to masks even when there were enough to go around, a state official said. The governor's office in mid-April directed hospitals to give a new N95 mask daily if a worker asked. That didn't universally happen, said the nurses' union, which filed the suit against the state's health department, saying it failed to "fulfill its mandate to protect the health of the public" and neglected to enforce guidelines around protective gear at hospitals. A state health-department spokesman, Gary Holmes, said: "Throughout this crisis we worked with our nurses and other front line heroes to make sure they had the proper equipment they needed amidst a world-wide shortage, and we were in constant contact with both union and hospitals to accomplish this." CLICK HERE TO READ MORE ON FOX BUSINESS Some workers said hospitals gave no clear policies on when N95 masks were considered soiled, and sometimes they only found out too late. Mikhail Migirov, a respiratory therapist at NewYork Presbyterian-Lower Manhattan, discovered his N95 was no longer fitting during an intubation when he was able to smell the patient's breath. "Oh my God," he said he thought. He later tested positive for Covid-19. NewYork-Presbyterian said staff were instructed to test the seals on their masks and request new masks if they were no longer safe. Scott Amrhein, a trade-association executive who helped procure PPE for nursing-home workers, became so distraught about the shortage of protective gear, among other issues nursing homes faced, that he died by suicide March 30, his son said. His father, he said, felt government officials had ignored him and the situation was getting worse for nursing homes, which were also now taking in Covid patients from overloaded hospitals. Mr. Amrhein was fielding hundreds of calls daily in late March from nursing homes and hadn't slept in weeks, said his son, Justin Amrhein. In emails to his friends and colleagues, the father said he didn't know how to slow the building disaster. "It is a travesty," the elder Mr. Amrhein wrote, "that our society and our leaders fail continuously — as now — to elevate, value and respect that critical work." –Joe Palazzolo, Melanie Grayce West, Jimmy Vielkind and Paul Berger contributed to this article. Source: Read Full Article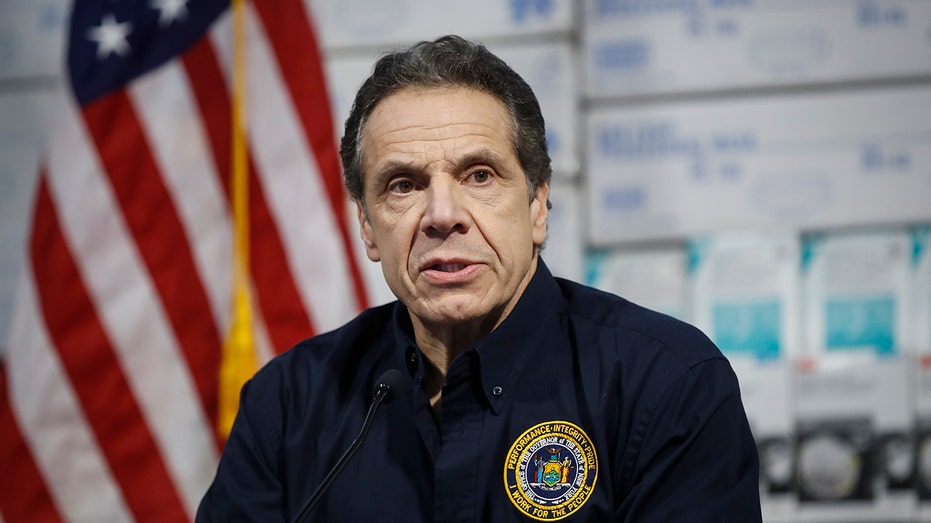

One planning lapse showed up in improper patient transfers. More than 1,600 largely Covid-19 patients in two of the state's largest hospital systems were moved from overloaded hospitals to ones less hit, according to spokespeople for those systems. Some patients arrived in worse condition than when they left, sometimes without names and treatment information, said doctors and nurses at several hospitals.
A Health + Hospitals spokeswoman, Stephanie Guzmán, said the city's 11-facility hospital system provided "the highest quality care to all New Yorkers." Only the least-sick patients were transferred between hospitals and their personal information was in a centralized system, she said.
