When you have a chronic condition, there’s the obvious physical toll, but there’s an equally daunting psychological one. What’s the secret to dealing with the impact on your mental health? Three men share what they’ve learned.
Dan Morris, 35: Crohn’s Disease

Dan Morris was in the middle of a classic Crohn’s flare but didn’t know it. All he knew was that his months-long bout of severe diarrhea was taking a toll. “I had lost a lot of weight to the point of looking skeletal,” says Morris, an online marketing professional based in Dunedin, Florida. “For some reason, it didn’t occur to me that I should go to a doctor until I was urged to by workmates.”
In the nine years since his diagnosis, Morris has come to understand that stress and Crohn’s—a type of inflammatory bowel disease that affects the lining of the digestive tract—exist on a two-way street. Not only does stress trigger flareups but living with the disease can be stressful.
“The physical and psychological impact are intertwined.”
“Both the physical and psychological impact of Crohn’s are intertwined,” says Morris, 35. “When things are going well physically, I’m free from anxiety and stress relating to the disease. I have been through years-long periods where I forget about it, and it feels like nothing is wrong with me.”
But then he’s hit with a reminder in the form of a flare-up and that’s when he’ll double down on the antidotes he’s accumulated over the years: Gardening, reading to his 3- and 5-year-old daughters, watching an episode or four of “The Office,” walking the family dog, carving out quiet time for spiritual reflection. “Another thing that helped during a recent flare was joining Crohn’s groups on Facebook,” says Morris. “It was really good to read what other people were going through so as not to feel alone.”
Michael Shelver, 26: Type 1 Diabetes

“The most stressful part about living with type 1 diabetes is that it is a 24-hour-a-day, seven-day-a-week, 365-days-a-year job,” says Michael Shelver, an exercise physiologist in San Jose, CA. “Managing a chronic condition, there are no days off, and sometimes you really, really need one. I’ve adopted the ‘pretty good, not perfect’ mindset. This is basically my realization that chasing perfect glucose management puts you on a mental and physical roller coaster that isn’t fun.”
It’s taken a while for Shelver to develop his “pretty good” approach to living with a chronic condition. As a teen, he regularly rebelled by taking days off from managing his diabetes. He’d let his blood glucose go unchecked to the point of having hypoglycemic seizures. “It was terrifying as a kid to be mentally processing the fact that every single day for the rest of my life I’ll be dealing with this,” says Shelver, now 26. “It makes you feel tremendously isolated from the general population that carries on day to day without the same worries.”
“It makes you feel tremendously isolated.”
It wasn’t until he found a community of teens also living with type 1, through a non-profit summer camp run by Diabetes Youth Families, that Shelver came to accept his diagnosis and change his view of lifelong management. Meeting people the same age facing the same condition and the same mental struggles, he says, he “was able to build confidence, consistency, and compassion in my diabetes management.”
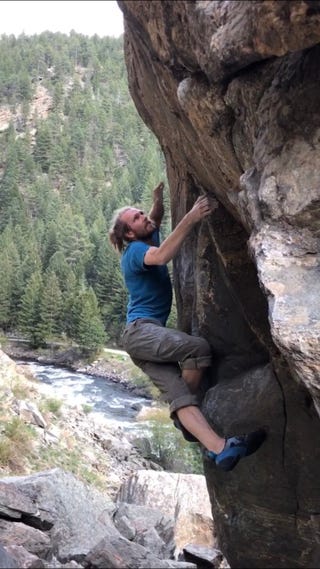
His number-one stress-reducer? Physical activity. “Getting my heart rate up with a run or pushing some weights in the gym improves my mood, sleep, and blood glucose,” he says. He also tries to limit technology and get outside as often as possible. “I love social media—it’s a powerful tool to connect with fellow adventurers and type 1s throughout the world,” he says. “It’s also a double-edged sword. You can find yourself digging into hours of highlight reels that only cause more stress.”
Two other reliable tools to help manage stress: Getting consistent, high-quality sleep and practicing mindfulness. “When I get stressed or angry or sad, I often ask myself ‘Why?’ to better understand what I can do to help myself,” says Shelver. “Mindfulness is a powerful tool, and I believe living with diabetes constantly sharpens that tool.”
Samuel Taylor, 26: Asthma
Samuel Taylor has battled asthma virtually his entire life. “Until the age of 10, trips to the hospital were a biweekly occurrence,” he says. In those days, “the stress wasn’t as omnipresent for me; more so for my parents. They were bearing the difficulty of paying for my care and fighting the anxiety of what might trigger my next attack.”
Although he battled depression throughout middle school and high school—the result of feeling like the only person in the world living with a chronic condition—he didn’t actively pursue ways to deal with the stress and anxiety until he was on his own. “There was a point, in my early college years, where I realized I can take steps to manage not only my asthma better but also my general health,” says Taylor, a public health professional in Denver, Colorado.
“It’s a ‘sink or swim’ lesson.”
To that end, he began practicing yoga and meditation. He also began tweaking his diet to limit his intake of foods high in histamines (like shellfish, dairy products, and processed meats) and focus more on nutrient-dense foods. He was almost instantly rewarded. That combination, he believes, led to a dramatic improvement in his asthma symptoms.
“What I have learned about managing stress is that it’s often a product of our perception; the more prepared we are for a stressful situation, the better our perception of the situation becomes,” says Taylor, 26. “Having a chronic condition isn’t easy. But it’s through challenges that we learn and managing the psychological impact of a chronic illness is a challenge. In a way, it’s a ‘sink or swim’ lesson, in which the consistent stress is a catalyst for vital growth of mental health maintenance skills.”
Source: Read Full Article
