*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
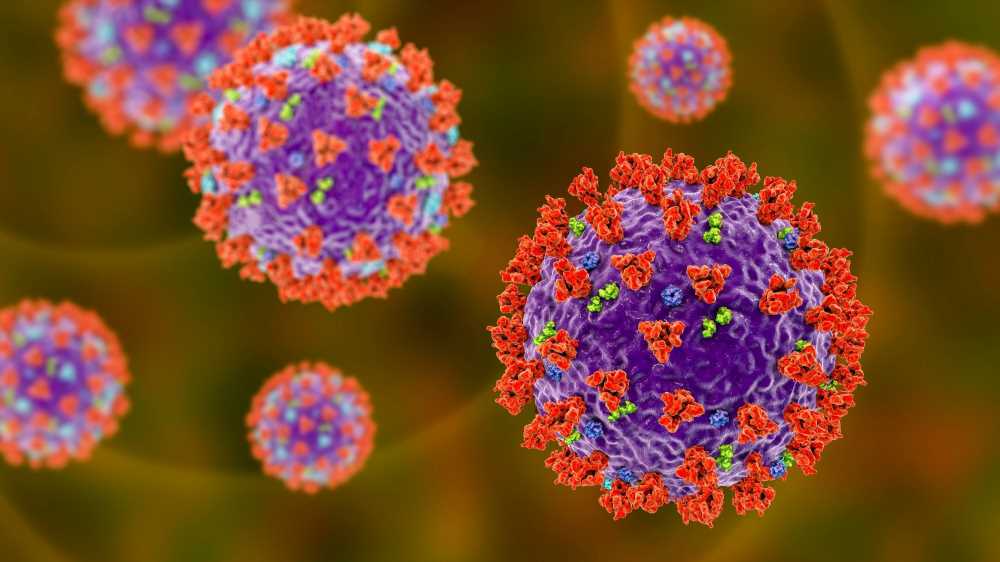
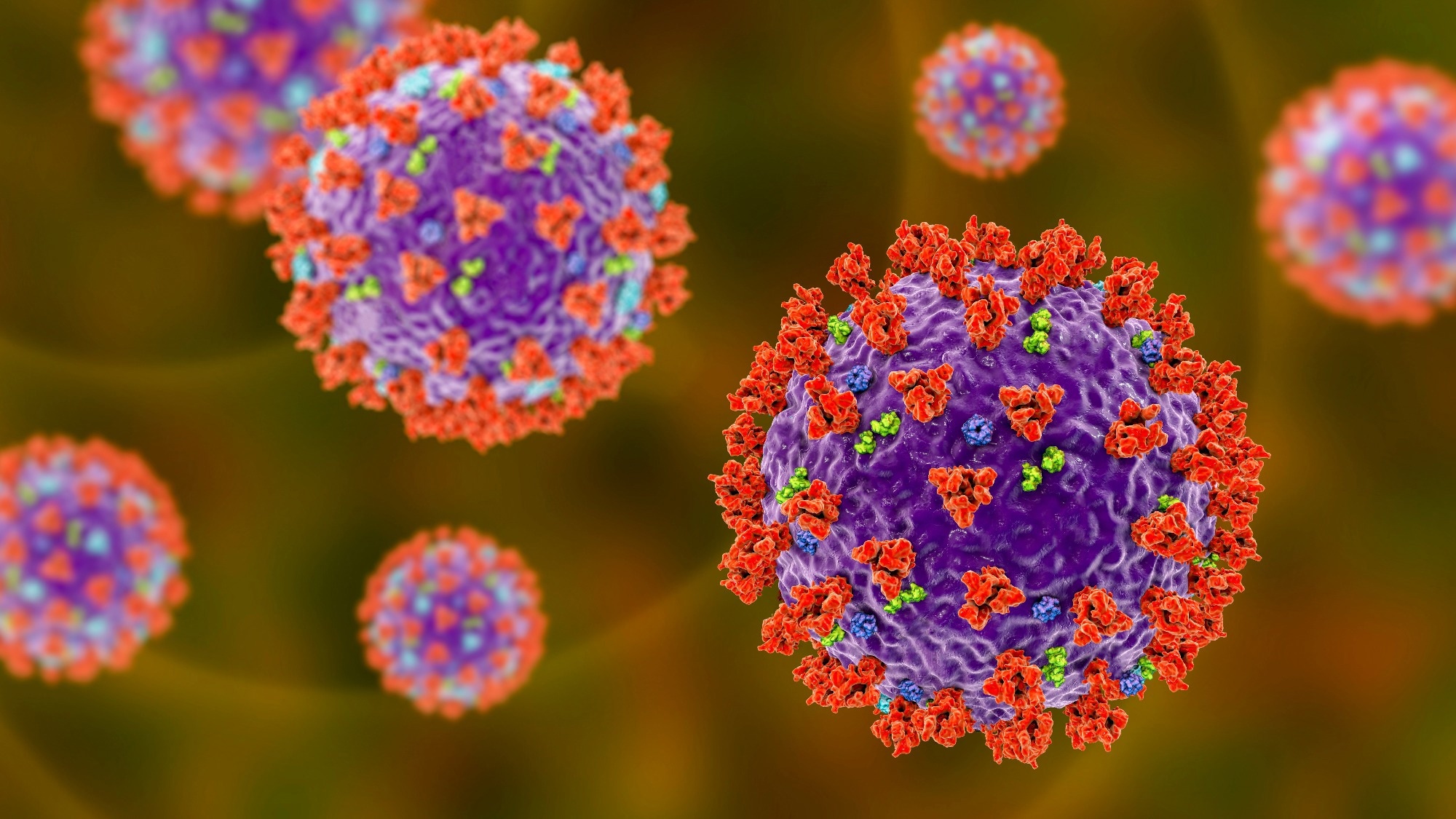
In a recent study posted to the bioRxiv* preprint server, researchers assessed the impact of evolutionary convergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) A-lineage (Clade 19B) spike sequences on B-lineage viral replication.
Immunology eBook
As of February 2023, the global transmission of coronavirus disease 2019 (COVID-19) has resulted in over 2000 novel phylogenetic assignments of named global outbreak (PANGO) lineages and 30 distinct Nextstrain clades. A minimum of two zoonotic events most likely triggered the division into two root viral lineages that were predominant in the initial three months of the pandemic- the more distantly related but earlier recognized B-lineages (Clade 19A) along with the more closely associated but later found A-lineages (Clade 19B) (Clade 19B). While there exists greater fidelity of SARS-CoV-2 genome replication due to the action of the exoribonuclease, mutations across the genome led to the emergence of the B.1-lineages (Clade 20A) with the selection of its characteristic D614G alteration in the SARS-CoV-2 spike gene.
About the study
In the present study, researchers characterized an early SARS-CoV-2 A-lineage variant A.3 along with three A.2.5 isolates with distinct mutations to determine their impact on the evolution of A.2.5 variants with B-lineage viruses in the viral spike gene.
In the period between early and mid-2021, the team found A.2.5 lineage variants as well as an A.23.1 variant corresponding to the timing of global A-lineage rebound at Johns Hopkins Hospital. The capability of the early A.3 lineage isolate and the later A.2.5 lineage isolate to evade neutralizing antibody responses was studied. Plaque reduction neutralization tests (PRNT) were performed on 10 COVID-19 convalescent plasma (CCP) specimens obtained from May 2020 to March 2021 against the four isolates. VeroE6 cells were subjected to plaque assays at 33°C as well as 37°C.
Plaque assays were performed on VeroE6-TMPRSS2-overexpressed cell monolayers to investigate the impacts of elevated expression of transmembrane serine protease 2 (TMPRSS2), which is a protease responsible for the processing and fusogenicity of the spike protein.
Results
Early A-lineage variants, including A, A.1, A.2.2, and A.3, were easily detectable up to mid-2020. A-lineages were not found until 2021, when A.2.5 variants arose. An A.3 strain called HP00076 and three A.2.5 strains called HP05922, VRLC091, and HP02153 were isolated from revealing that the A.2.5 viruses had accumulated mutations across their genomes in comparison to A.3, with each of these isolates encoding a distinct mutation profile. A.2.5 isolates displayed a minimum of five conserved spike mutations, including D215A, 141-143, L452R, D614G, and ins215AGY. Notably, VRLC091 exhibited three substitutions of W152R, A263S, and T240I. These mutations, which were also present in other VOCs, indicated convergent evolution between A.2.5 variations and the spike sequences of SARS-CoV-2 variants of concern (VOCs).
All three A.2.5 lineage viruses exhibited a 2.5- to 5-fold decrease in geometric mean half-maximal inhibitory concentration titer (GMT) compared to A.3 isolates, indicating a greater ability to evade neutralization. This suggested that A.2.5 isolates have adapted to largely evade neutralizing activity developed against viruses that were in circulation during the same time period.
By 96 hours post-infection (hpi) at 37°C and 120hpi at 33°C, the four isolates produced countable opaque plaques. Assessing and comparing plaque areas at 37°C demonstrated that the three A.2.5 isolates produced plaques with smaller mean diameters than the A.3 isolate HP00076. Furthermore, the mean plaque areas of A.2.5 isolates were 1.5 to 2.6 times lesser than those of A.3, with VLRC091 producing the largest plaques among A.2.5 isolates. On the other hand, at 33°C, all the A.2.5 isolates produced plaques significantly smaller than HP00076, and between 2.2 and 3.5 times smaller than A3.
As opposed to the opaque plaques observed on VeroE6 cells, at 48hpi at 37°C and 72hpi at 33°C, all of the isolates developed transparent and distinctly recognizable plaques. Plaques formed faster on VeroE6-TMPRSS2 cells than on wild-type VeroE6 cells, however, at both temperatures, A.2.5 isolates formed plaques that were smaller than A.3 isolates. Plaques of A.2.5 isolates were 2.6- to 3-fold smaller than those of A.3 at 37°C. At 33°C, the plaques of A.2.5 isolates were 2.3- to 4.4-fold smaller than the A.3 plaques.
At 37°C, a distinct growth difference was noted, with A.2.5 isolates growing faster than A.3 and generating about 10-fold greater peak titers, albeit peaking at roughly the same time for all isolates. The average peak titer of HP00076 was lower than that of HP02153, HP05922, and VRLC091. All A.2.5 isolates generated more total infectious virus than A.3 isolates, among which HP00076 displayed the highest AUC compared to HP05922, VRLC091, and HP02153.
Conclusion
The study findings showed that infectious clone technologies could be utilized to discover the mutations responsible for changes in viral features such as proliferation in primary human nasal epithelial cells, syncytia formation, and neutralization escape likely caused by spike mutations. However, the observations of A.2.5 neutralization escape from circulating, pre-existing immunity, and overall increased replication capacities in human nasal epithelial cell cultures suggest the re-emergence of SARS-CoV-2 A-lineage variants.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Preliminary scientific report. Steve Yoon, Eduardo U. Anaya, Jaiprasath Sachithanandham, Benjamin A. Pinsky, David J Sullivan, Heba H Mostafa, Andrew Pekosz. (2023). Convergent Evolution of A-Lineage (Clade 19B) SARS-CoV-2 Spike Sequences with B-Lineage Variants of Concern Affects Virus Replication in a Temperature-Dependent Manner on Human Nasal Epithelial Cell Cultures. bioRxiv. doi: https://doi.org/10.1101/2023.03.03.531067 https://www.biorxiv.org/content/10.1101/2023.03.03.531067v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibody, Cell, Convalescent Plasma, Coronavirus, Coronavirus Disease COVID-19, covid-19, Evolution, Gene, Genome, Hospital, immunity, Mutation, Pandemic, Proliferation, Protein, Respiratory, SARS, SARS-CoV-2, Serine, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Virus

Written by
Bhavana Kunkalikar
Bhavana Kunkalikar is a medical writer based in Goa, India. Her academic background is in Pharmaceutical sciences and she holds a Bachelor's degree in Pharmacy. Her educational background allowed her to foster an interest in anatomical and physiological sciences. Her college project work based on ‘The manifestations and causes of sickle cell anemia’ formed the stepping stone to a life-long fascination with human pathophysiology.
Source: Read Full Article