Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection causes a "cytokine storm" in hospitalized and ICU patients. Studies have shown that the blockade of cytokine signaling and steroid treatment helps achieve positive outcomes in patients. However, a better understanding of the downstream signaling pathways contributing to the massive immune response is crucial to treat patients suffering from severe COVID-19 symptoms.
Analyzing the response of COVID-19 relevant cell types to inflammatory cytokines released during the cytokine storm
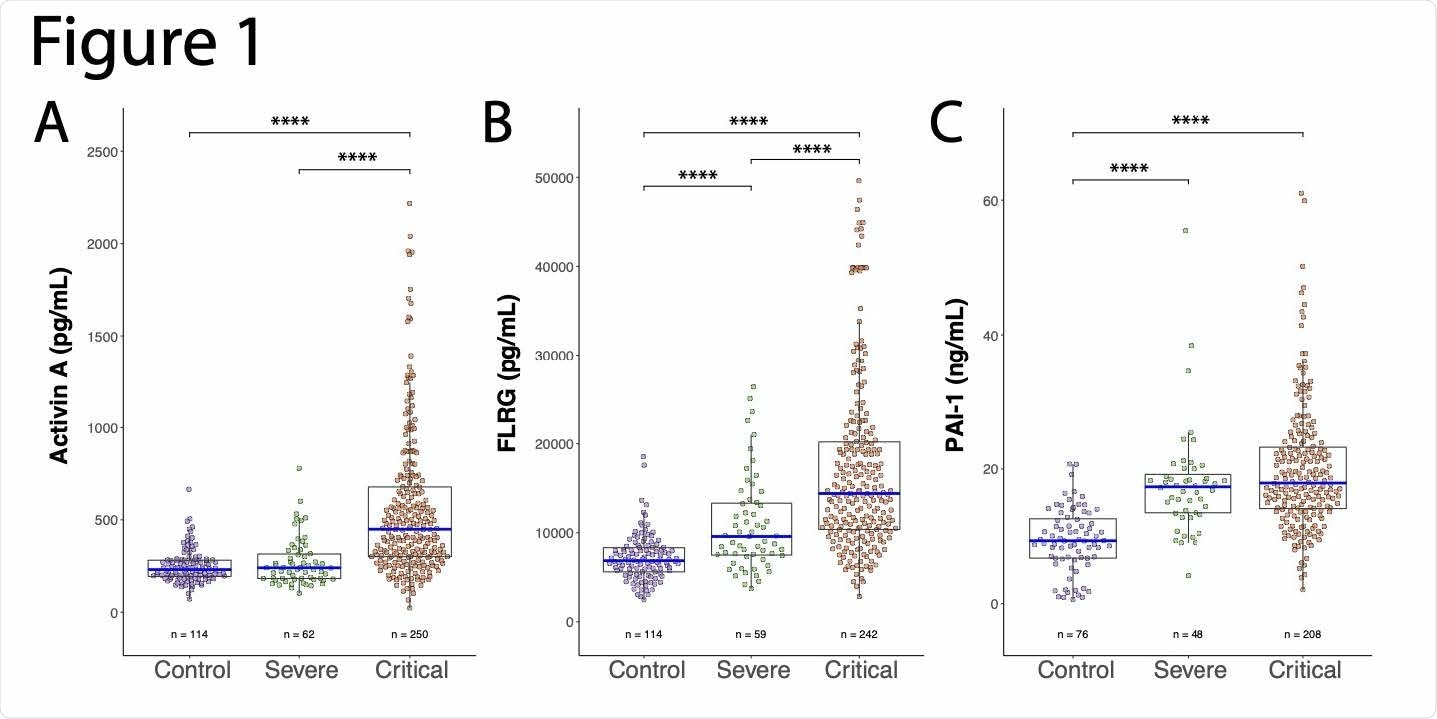
Recently researchers from the US studied serum from COVID-19 patients to see if they had elevated Activin A levels. They also evaluated PAI-1, another marker found to be associated with ARDS, and one of the parameters said to be associated with ARDS-related mortality. They further determined if the levels of Activin A, follistatin-like related gene (FLRG) and PAI correlated to key COVID-19 disease markers such as the supplemental oxygen requirement, ARDS symptoms, and mortality. The study is published on the preprint server bioRxiv*.
The researchers had previously analyzed IL-1 and TNFα in the setting of skeletal muscle cachexia, where the cytokines induce skeletal muscle atrophy. They learned from their previous studies that IL-1 and TNFα could induce Activin A production in skeletal muscles, which induces skeletal muscle atrophy. They felt that this was relevant in the context of COVID-19, and it had been previously reported. Earlier, it has been reported that high levels of Activin A were found in the bronchial alveolar lavage fluid of patients who had acute respiratory disease syndrome (ARDS).
"The impression, therefore, is that these severely affected patients are not suffering directly from the viral load, but instead from an over-reaction of the immune system – the later occurring cytokine response, which in some patients over-induces Activin A."
Elevated levels of Activin A and FLRG at baseline were predictors of the severe COVID-19 outcomes
In the present study, the researchers wanted to see if other COVID-19 relevant cell types such as bronchial and pulmonary smooth muscles responded in a similar manner to inflammatory cytokines released during the cytokine storm to produce Activin A. They had performed a trial with COVID-19 patients using a Regeneron anti-IL-6R antibody in which they evaluated the serum of these patients post-randomization and before therapy to measure baseline Activin A, PAI-1, and FLRG levels. They then correlated these values to baseline clinical and lab variables and key disease outcomes.
The study results demonstrated that cytokines responsible for activating the NF-kappaβ pathway could also induce Activin A and its downstream marker, FLRG. In hospitalized COVID-19 patients, high levels of Activin A / FLRG at baseline were predictors of the severe COVID-19 outcomes, such as the need for ventilation and all-cause mortality. Patients with higher than median levels of Activin A / FLRG were nearly three times more likely to die compared to patients who had Activin A / FLRG levels below the sample median.
Inhibiting Activin A can be beneficial in the treatment of COVID-19 patients experiencing ARDS
The findings demonstrate that both Activin A and FLRG were significantly upregulated in COVID-19 patients in the ICU. Some patients experienced an over 2-fold increase in Activin A. Interestingly, Activin A levels were not significantly increased in severe COVID-19 patients who did not require invasive mechanical ventilation showing that the marker can clearly distinguish the patient populations.
While FLRG levels increased in patients with severe disease who were not in the ICU, it was even more elevated in ICU patients, especially those who had ARDS and needed invasive mechanical ventilation. Additionally, subjects with extremely high increases of FLRG were also found to be more likely to need invasive ventilation. Thus, high levels of Activin A and FLRG increases the risk of ARDS in COVID-19 patients, and the blockade of Activin A can be beneficial in the treatment of COVID-19 patients experiencing ARDS.
"We, therefore, suggest it's reasonable to try inhibiting Activin A or its induced pathway to treat COVID-19 patients who are experiencing ARDS."
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Activin A correlates with the worst outcomes in COVID-19 patients, and can be induced by cytokines via the IKK/NF-kappa B pathway Megan McAleavy, Qian Zhang, Jianing Xu, Li Pan, Matthew Wakai, Peter J. Ehmann, Matthew F. Wipperman, Tea Shavlakadze, Sara C. Hamon, Anita Boyapati, Lori G. Morton, Christos A. Kyratsous, David J. Glass, bioRxiv, 2021.02.04.429815; doi: https://doi.org/10.1101/2021.02.04.429815, https://www.biorxiv.org/content/10.1101/2021.02.04.429815v1
Posted in: Medical Research News | Disease/Infection News
Tags: Antibody, Cachexia, Cell, Coronavirus, Coronavirus Disease COVID-19, Cytokine, Cytokines, Gene, Immune Response, Immune System, Mortality, Muscle, Muscle Atrophy, Oxygen, Respiratory, Respiratory Disease, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Steroid, Syndrome

Written by
Susha Cheriyedath
Susha has a Bachelor of Science (B.Sc.) degree in Chemistry and Master of Science (M.Sc) degree in Biochemistry from the University of Calicut, India. She always had a keen interest in medical and health science. As part of her masters degree, she specialized in Biochemistry, with an emphasis on Microbiology, Physiology, Biotechnology, and Nutrition. In her spare time, she loves to cook up a storm in the kitchen with her super-messy baking experiments.
Source: Read Full Article
