The coronavirus disease 2019 (COVID-19) pandemic caused millions of deaths throughout the world, which has provoked intense research into the pathogenetic mechanism behind this disease.
A new study published on the medRxiv* preprint reports finds very low aldosterone levels in a subset of COVID-19 patients, thereby pointing to the involvement of renal hormones in the immunothrombotic and inflammatory phenomena typically seen in severe COVID-19.
Study: Unquantifiably Low Aldosterone Concentrations Are Prevalent in Hospitalised Covid-19 Patients but May Not Be Revealed By Chemiluminescent Immunoassay. Image Credit: Kateryna Kon / Shutterstock.com
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the pathogen responsible for COVID-19, binds to the angiotensin-converting enzyme 2 (ACE2) receptor to gain entry into the host cell. The ACE2 receptor is also a key component of the renin-angiotensin-aldosterone system (RAAS), which regulates renal and cardiovascular function in many ways.
ACE2 converts angiotensin II (AngII) to the anti-inflammatory and vasodilator antioxidant molecule Angiotensin 1-7 (Ang1-7), which allows for the inhibition of RAAS. Conversely, AngII is a powerful vasoconstrictor, pro-oxidant, and pro-inflammatory molecule that may also trigger fibrosis, aberrant coagulation, and immunothrombosis through its effect on the endothelium. This activity is mediated by endothelial production of tissue factor and plasminogen activator inhibitor 1.
AngII also binds the adrenal angiotensin I receptor, which leads to the production of aldosterone, the major mineralocorticoid in the body. By binding with ACE2 and thus blocking AngII metabolism, SARS-CoV-2 can activate the RAAS and promote high aldosterone secretion. The excessive AngII activity may contribute to hypertension, thrombosis, inflammation, and lung fibrosis in COVID-19.
Earlier studies have failed to demonstrate RAAS activation or low aldosterone levels; however, these studies often used non-specific methods that are very vulnerable to interference. For this reason, the researchers of the current study used mass spectrometry, as it is devoid of interference and provides more accurate estimates.
Earlier, the scientists had several patients with low aldosterone, though this has not been reported as typical. In order to further examine this observation, the researchers used liquid chromatography-tandem mass spectrometry (LC-MS) to estimate aldosterone levels in hospitalized COVID-19 patients.
Study findings
All patients had tested positive for SARS-CoV-2, all of which had a median age of 64 years. Of 134 patients with baseline aldosterone, cortisol, or renin levels within 72 hours of the first positive test for SARS-CoV-2, about 60% were male. About 11% of the patients were administered to the intensive care unit (ICU), with an in-hospital mortality rate of 13.4%.
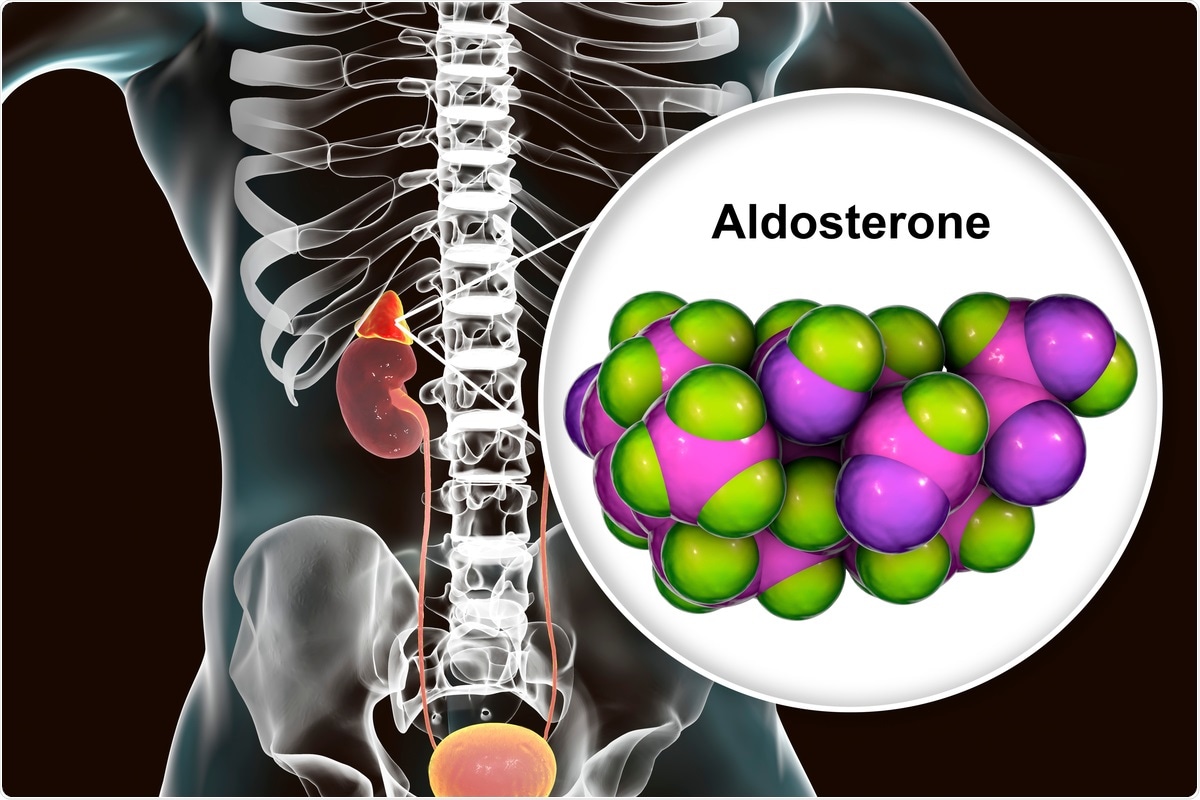
Aldosterone concentrations were very low, with almost 60% having undetectable aldosterone levels below 70 pmol/L. Cortisol was higher than 744 nmol/L in 20.5% of patients, which represented the discriminant between survival and non-survival curves in earlier studies.
Renin concentrations were also typically low, even though aldosterone levels were reduced, which would normally have increased renin levels. Aldosterone levels were correlated with cortisol and renin concentrations; however, the lack of detectable aldosterone was not a marker for any clinical feature or outcome, survival, or renal function.
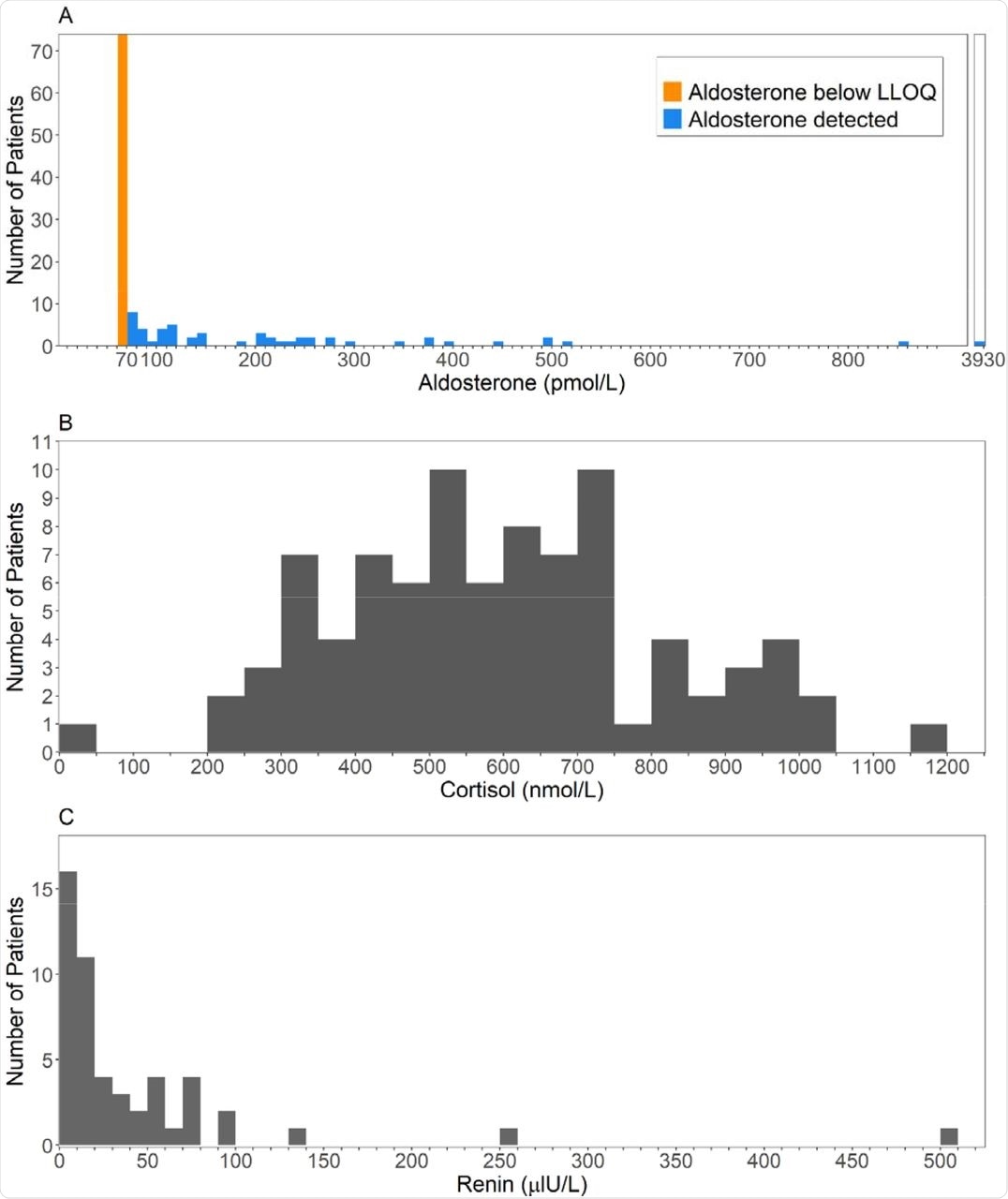
Histograms of the first available result (A) Aldosterone, measured using LCMSMS (B) Cortisol (C) Renin.
High cortisol levels exceeding 744 nmol/L were linked to lower survival odds as compared to those with lower levels. That is, 44% of those in the former group died by 28 days as compared to 11% in the low cortisol group. Moreover, the high-cortisol cohort had a mean hospital stay of 19 days as compared to 11 days in the low-cortisol group.
A marked difference in survival was seen when cortisol levels exceeded 800 nmol/L in the high cortisol group.
Earlier studies that used immunoassay methods to measure aldosterone levels failed to find any significant change in COVID-19 patients as compared to controls. The very different results with this study are attributed to the use of LC-MS. When the measurements were repeated by chemiluminescent immunoassay (CLIA), they found that CLIA (pmol/L) = 14.1 + 3.16 × LC-MS (pmol/L).
Thus, there is a major variation in the results obtained by these methods, which only increases as the mean measurements increase. These differences are not explained by altered renal or liver function.
However, if the serum was subjected to solvent extraction, the results came into much closer agreement, where Extracted CLIA = -14.9 + 1.0 × LC-MS. This is explained by the presence of a water-soluble metabolite that interferes with the substance to be detected in the immunoassay.
Implications
The absence of clinical features of hypoaldosteronism has given rise to many hypotheses, including adequate mineralocorticoid activity to maintain the homeostasis of water and electrolytes. High cortisol levels may act at the mineralocorticoid receptor (MR), since the inactivating enzyme 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2) is saturated at these levels, thereby allowing glucocorticoid-MR crosstalk.
This may explain the lack of hypoaldosteronism clinically, but only in part because of the reduced correlation between cortisol and aldosterone levels in these patients. Aldosterone metabolites also do not appear to bind very strongly to the MR, thus ruling out their compensatory action.
Alternatively, the activity of distal nephron epithelial sodium channels (EnaC) by AngII leads to increased reabsorption of sodium and an increase in blood volume, though potassium and hydrogen ions are excreted at a higher rate. This could initiate a vicious negative-feedback cycle for the RAAS, where renin and aldosterone levels fall further, even as AngII activity continues to be excessive due to the lack of ACE2 inhibition.
The poor agreement between CLIA and LC-MS corroborates earlier studies while showing that COVID-19 exacerbates this issue. Solvent extraction probably eliminates a water-soluble metabolite that cross-reacts in the immunoassay. The prime candidate is the predominant aldosterone metabolite, aldosterone-18-glucuronide.
These data demonstrate that aldosterone cannot be accurately estimated in serum from patients with SARS-CoV-2 infection using direct competitive immunoassay. When measured using gold-standard LCMSMS, serum aldosterone is found to be remarkably low in most patients with COVID-19.”
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Wiegand, M., Halsall, D. J., Cowan, S. L., et al. (2022). Unquantifiably Low Aldosterone Concentrations Are Prevalent in Hospitalised Covid-19 Patients but May Not Be Revealed By Chemiluminescent Immunoassay. medRxiv. doi:10.1101/2022.02.28.22271645. https://www.medrxiv.org/content/10.1101/2022.02.28.22271645v1.
Posted in: Chromatography | Medical Research News | Medical Condition News | Disease/Infection News
Tags: ACE2, Aldosterone, Angiotensin, Angiotensin-Converting Enzyme 2, Anti-Inflammatory, Antioxidant, Blood, Cell, Chromatography, Coronavirus, Coronavirus Disease COVID-19, Cortisol, Enzyme, Fibrosis, Glucocorticoid, Hospital, Immunoassay, Inflammation, Intensive Care, Liquid Chromatography, Liver, Mass Spectrometry, Metabolism, Metabolite, Metabolites, Molecule, Mortality, Pandemic, Pathogen, Potassium, Receptor, Renin, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spectrometry, Syndrome, Thrombosis

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article