The availability of rapid, accessible testing was integral to overcoming the worst surges of the COVID-19 pandemic, and will be necessary to keep up with emerging variants. However, these tests come with unfortunate costs.
Polymerase chain reaction (PCR) tests, the “gold standard” for diagnostic testing, are hampered by waste. They require significant time (results can take up to a day or more) as well as specialized equipment and labor, all of which increase costs.
The sophistication of PCR tests makes them harder to tweak, and therefore slower to respond to new variants. They also carry environmental impacts. For example, most biosensor tests developed to date use printed circuit boards, or PCBs, the same materials used in computers. PCBs are difficult to recycle and slow to biodegrade, using large amounts of metal, plastic and non-eco-friendly materials.
In addition, most PCR tests end up in landfills, resulting in material waste and secondary contamination. An analysis by the World Health Organization (WHO) estimated that, as of February 2022, “over 140 million test kits, with a potential to generate 2,600 tons of non-infectious waste (mainly plastic) and 731,000 liters of chemical waste (equivalent to one-third of an Olympic-size swimming pool) have been shipped.”
In order to balance the need for fast, affordable and accurate testing while addressing these environmental concerns, César de la Fuente, Presidential Assistant Professor in Bioengineering and Chemical and Biomolecular Engineering in the School of Engineering and Applied Science, with additional primary appointments in Psychiatry and Microbiology within the Perelman School of Medicine, has turned his attention to the urgent need for “green” testing materials.
The de la Fuente lab has been working on creative ways to create faster and cheaper testing for COVID-19 since the outbreak of the pandemic. Utilizing his lab’s focus on machine biology and the treatment of infectious disease, they created RAPID, an aptly named test that generates results in minutes with a high degree of accuracy. An even more cost-effective version, called LEAD, was created using electrodes made from graphite. A third test, called COLOR, was a low-cost optodiagnostic test printed on cotton swabs.
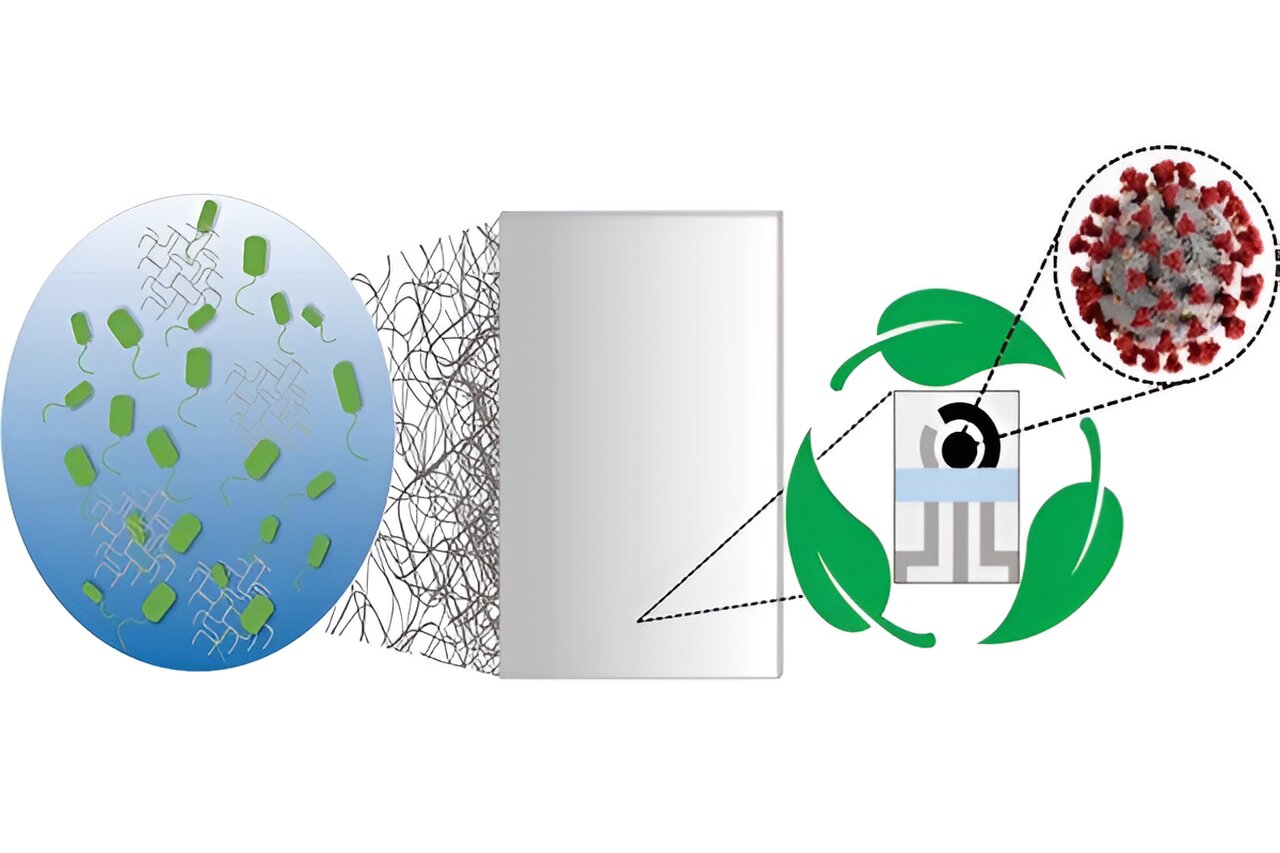
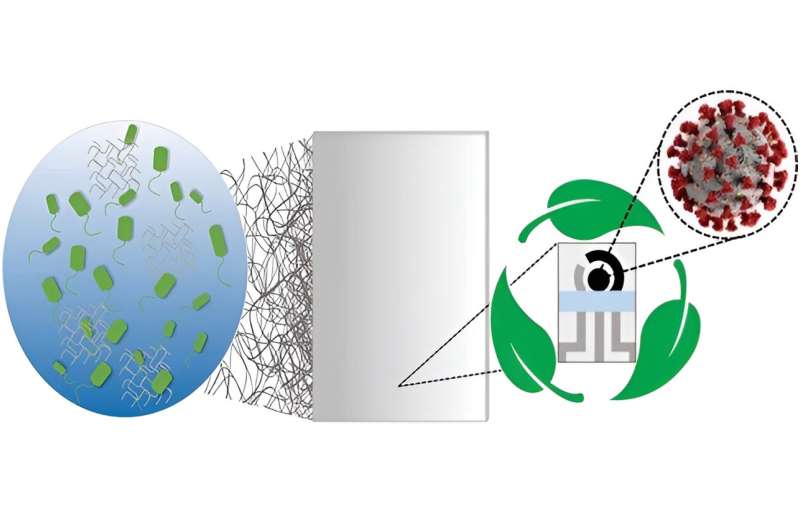
The team’s latest innovation incorporates the speed and cost-effectiveness of previous tests with eco-friendly materials. In a paper published in Cell Reports Physical Science, the group introduces a new test made from bacterial cellulose (BC), an organic compound synthesized from several strains of bacteria, as a substitute for PCBs.
Bacteria naturally serves as a “factory” for the production of cellulose, a paper-like substance which can be used as the basis for biosensors. BC is highly versatile, having been used for wound care, regenerative medicine and point-of-care or POC diagnostics. POC testing is especially important for the prevention of pandemics, in that it allows for quick and accurate diagnostics at the testing site without the need for expensive, specialized equipment or for the samples to be sent away to a lab.
This new BC test is non-toxic, naturally biodegradable and both inexpensive and scalable to mass production, currently costing less than $4.00 per test to produce. Its cellulose fibers do not require the chemicals used to manufacture paper, and the test is almost entirely biodegradable. (The exception is a small amount of silver, which can be easily removed and recycled by health care professionals.)
In addition to these green benefits, the test proved highly accurate in clinical trials, correctly identifying multiple variants in under ten minutes. This means that the tests won’t require “recalibration” to accurately test for new variants.
For de la Fuente, this new COVID test is one step in a wider movement toward “responsible innovation.”
“There’s a tension between these two worlds of innovation and conservation,” he says. “When we create new technology, we have a responsibility to think through the consequences for the planet and to find ways to mitigate the environmental impact.”
Beyond the contributions this test can make to the ongoing fight against COVID-19, de la Fuente’s higher aspirations are to find green alternatives for diagnostic testing broadly.
“There is a need for biodegradable diagnostic testing,” he says. “We will be continuing to perfect this technology, which could hopefully help many people in the future, while also looking to expand it to other emerging pathogens in anticipation of future pandemics.”
This study was an international collaboration between the de la Fuente lab and William Reis De Araujo, professor in analytical chemistry at the University of Campinas (UNICAMP) in São Paulo, Brazil, who leads the Portable Chemical Sensors Lab. The two teams have collaborated for years, with De Araujo’s expertise in electrochemistry complementing the diverse and interdisciplinary interests of the de la Fuente lab.
As researchers and health care providers continue to manage the effects of COVID-19, and look ahead to the prevention of future pandemics, inexpensive and accurate testing that is also environmentally friendly is crucial to protecting the health of both our planet and its people. The results of this study suggest that these goals need not be mutually exclusive.
More information:
Lucas F. de Lima et al, A bacterial cellulose-based and low-cost electrochemical biosensor for ultrasensitive detection of SARS-CoV-2, Cell Reports Physical Science (2023). DOI: 10.1016/j.xcrp.2023.101476
Journal information:
Cell Reports Physical Science
Source: Read Full Article